Blog
December 25, 2025
The Periodic Table of Data
Sitting by the fire this Christmas morning thinking about data governance systems (DGS), and I couldn’t help but visualize raw data (or “original records” in GXP language) as elements in the periodic table. That periodic table is what hooked me as a kid on the scientific path. It was a turning point for me, as everything we see, taste, smell and even think is based on various combinations of these basic elements combining and interacting in truly impressive fashion. It’s amazing…
We might think of raw data within our organizations in a similar manner. Every action we take, decision we make, and corporate strategy we implement should be based on the exact same pattern of combination and interaction. The problem is most of our data remains in the “periodic table” format – with few combinations and interactions. We see data as individual elements in the table, and then make decisions largely on ‘theory’ of what the data is telling us. The problem here is that theory is not the most effective way of making scientific judgements surrounding medical products. Best would be to run the experiment – see how the data ‘combines and reacts’ through analysis and/or visualization.
One of the earliest and simplest visualization tools is the control chart, thought to have been first used extensively in the 1920’s at Bell Telephone Laboratories. This tool uses two elements (e.g., defects vs. date) and combines these elements together to form a more complex compound that can perform some useful function for quality and the business, such as hydrogen and oxygen combining to form water – which has incredible function. Alone, these elements have little function in the world, but combined they change everything. Finding the most useful combinations in our data sets can result in function, and putting these functions to work through continuous improvement is what will separate the great companies of the next generation from the rest. But how do you do it?
Data Value via the DGS. From data -> risk -> value using the tools outlined in ICH Q8, Q9 and Q10. Are you ready?
Pete
December 22, 2025
The DGS Experience
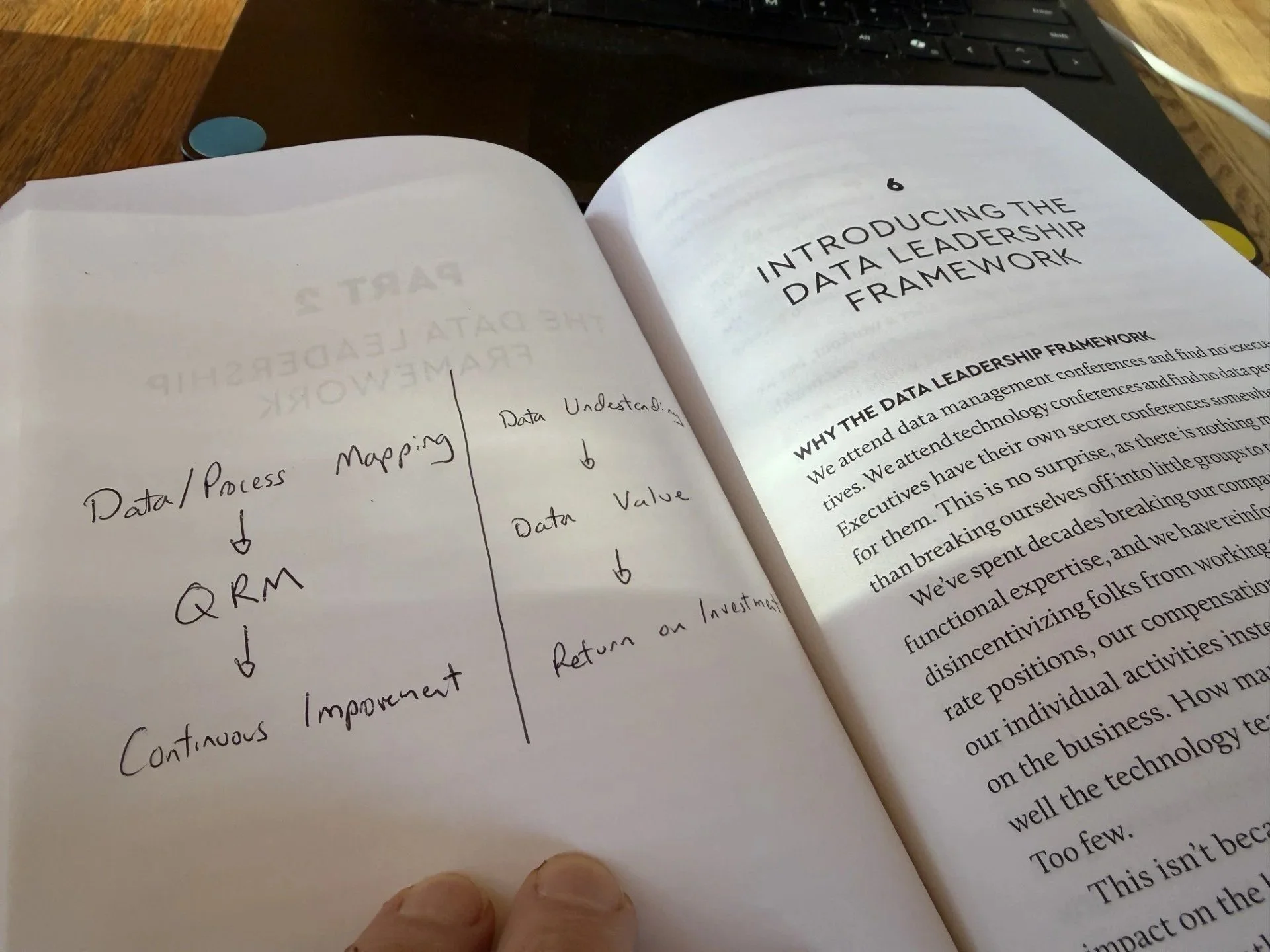
It’s a beautiful day here in Southern Colorado, and I spent the morning in front of the fire reading chapter 6 of one of my favorite books on data governance: “Data Leadership for Everyone” – Anthony J. Algmin. If you haven’t had a chance to read it – I highly recommend bumping it up on your 2026 queue!
Chapter 6 [and really the book in general] speaks to the fact that data governance without leadership and a clear goal to establish ROI assures failure. This takes vision and planning. The most important ingredient in a data governance system (DGS) is not actually the data… Data is needed [obviously], but the most important factor is establishing ‘data value’ and ROI through people’s participation in the DGS. If no beneficial actions come from the DGS (other than some “compliance satisfaction”) and passing an internal audit, then the whole thing was a massive capital sink and will forgotten by 2027. The term DGS will be viewed as negatively as the ALCOA project, which began in 2015 and piled layers of additional work on our operations staff with little ROI from the quality or business perspective.
Success in our next endeavor (the DGS) will require a mix of senior leaders, middle managers and front-line operations staff all establishing a common aim other than “compliance”. In the GXP world, a DGS is not optional, as it is explicitly expected per the EU GMP Chapter 4 [revision] – but what is a DGS?
A DGS is a theory… a way of thinking and acting that goes way beyond SOPs and compliance training. It requires top management to establish a common aim throughout the organization: continuous improvement, which is then executed throughout the organization through the GXP framework: establish the meaning/value of our data (ICH Q9) and then act on that data (CAPA) to make a better product at a lower cost… this also happens also to align perfectly with patient safety – hence in theory this should be an easy adjustment for us in the GXP universe. But I am 100% convinced that this will depend on your senior leadership. As I have mentioned previously in this blog, if you want to enjoy meaning in labor and a great place to work, make sure your leadership is aligned with this goal – otherwise get your resume out there. It is not your job to convince management that a DGS is a worthwhile endeavor. Who wants to swim through the swamp of patchwork CAPAs, never ending deviations, and metrics that are designed to place blame on employees instead of leaders?
There are various levels of a functioning DGS, from basic to advanced. Any organization can establish a fake DGS for regulatory inspection, where beautiful SOPs written by consultants shine brightly from the screen in the conference room, perhaps even a fancy PPT is presented with AI generated images and buzz words… The inspector is initially impressed, but then disappointed once they realize data remains siloed and individual departments struggle to understand what to do with all these audit trails and how they are at all connected to the product/patient. Some days, if they don’t have time – they just skip the review… I fully understand. Don’t ask me to perform a task without understanding the meaning – that is dehumanizing.
The goal of a DGS as outlined in the GMP regulation was never intended to be a “compliance activity” – like old school 1970’s regulations… This is a new era of regulation, where requirements are aligned with good practices from other industries who make excellent products at low costs and have high levels of worker satisfaction in labor.
To get started here are three simple bullets that summarize the journey as outlined in our GXP guidance and regulation:
Data/Process Mapping
Data/Process Risk Assessment
This exercise establishes “data value”
What to review, how often, and its importance
Continuous Improvement via CAPA
This demonstrates ROI from the DGS and engages employees… without continuous improvement as the final step: expected and measured [metrics] by senior leaders, the DGS will wilt faster than a flower in the desert
Once your senior leaders have established the end goal of the DGS, and have provided usable tools and clear metrics – the project can get started and will accelerate quickly; with success [almost] guaranteed.
Pete
November 27, 2025
When to CAPA?
This is an age-old question that has introduced serious confusion and difficulties for GMP generations, and is highlighted within this FDA Form 483 from early 2025. Let’s discuss a new & modern strategy in this blog entry…
In a modern quality system, a CAPA should never be initiated without sound scientific rationale, which can be found in a documented risk assessment. This risk assessment is key. Process/workflow changes can be disruptive, require extensive re-training of staff, and introduce confusion when requirements are continuously altered within daily routine tasks. The result is an increase in mistakes; the opposite desired outcome.
So… when is a CAPA deemed necessary? This really depends on the maturity of the site’s Quality System. For example, if detailed workflow-level risk assessments have been established, predicting errors along with an assessment of risk (severity * vulnerability), CAPAs should be reserved only for systemic, repetitive, or high-severity errors. In all other cases, [which make up the vast majority of our deviations], mistakes (deviations) may be considered common-cause (we knew that was going to happen based on vulnerabilities within the workflow). A CAPA may not be required when low-severity errors occur, unless a trend or widespread scope is identified.
Common-cause variation could be defined as “the inherent, random, and predictable fluctuation that exists in any process due to its design.” I argue that this predictable fluctuation also applies to human errors, which are likely the largest category of deviations within your program. If we have identified and assessed potential human factor hazards and proactively determined the impact of such errors (e.g., low/medium/high), and regularly trend such errors with granularity, we have sound scientific rationale available during the FDA inspection to justify no CAPA.
In the FDA Form 483 example above, the site would have needed to provide the investigator with the scientific rationale to justify no CAPA; with that rationale demonstrating that the error did not fall into one of the three categories mentioned above (systemic, repetitive, high-severity). But without that… no dice. It is of critical importance that the site grasps the difference between a proactive and reactive risk assessment. In a modern quality system, proactive risk assessments are available to demonstrate a state of control (validation), and then utilized as a base for reactive risk assessments performed during the deviation exercise. Note that the severity dimension of risk is utilized as the primary factor when evaluating the need for a CAPA. If a CAPA is then deemed necessary, the site has 3 primary options, arranged here in order of priority: 1) re-design the hazard out of the workflow, 2) reduce the vulnerability dimension via the addition of technical/engineering solutions, or 3) simplify and streamline. But…. where does this leave the addition of procedural controls, you might ask? These are a last resort and should be avoided whenever possible as they do not reduce vulnerability - a more likely means to reduce mistakes is via simplification and streamlining as outlined in option #3, even though vulnerability of the hazard occurring remains the same.
Without a proactive quality system established with comprehensive workflow-level risk assessments, however, it may be impossible to demonstrate such rationale within each deviation record due to limited resources/time – hence a burdensome reactive quality system emerges where CAPAs are always required for any error regardless of their risk, scope and/or frequency, because the site has no other option available. This is a sad situation, and makes it nearly impossible for the site to achieve its common aim – with heavy waste incurred as folks scramble with re-trainings, more errors, and employee disengagement.
Pete
November 22, 2025
Simplify and Streamline
Human-related mistakes during production or testing can often lead to loss in confidence in GXP data sets. Sometimes, these result in product recall, regulatory action, drug shortage, or other consequences we would very much like to avoid. Most mistakes are concentrated in those areas of our processes that are highly manual and rely on the ability of the human to perform the action “right first time”, often within a high-pressure environment with multiple and continuous distractions. As a result, we have implemented the concept of “witnessing” or “verification” to reduce the risk that any mistake will go undetected. In theory, this makes total sense – but in reality, I have my doubts. Let’s break it down:
First and foremost, in my experience most companies do not have nearly enough resources to honestly perform the amount of witnessing required per their procedures. As a result, “witnessing” becomes a compliance activity that holds little value, and is the first thing to be skipped when the pressure is on (Friday afternoon?). When detected by a regulator, this is considered ‘falsification’ or records, a serious charge that questions the documentation throughout the entire site – as it will likely be interpreted as a cultural practice (think ‘iceberg analogy’).
Secondly, a witness does not realistically reduce the risk of a mistake occurring, only the ability to [maybe] detect a mistake as it occurs. “Maybe” is the reality – due to the first point -> lack of resources. It is unlikely that the witness has the time/energy to catch the mistake as it happens, therefore witnessing becomes a compliance formality rather than a meaningful activity. So the question is: what value does it bring to achieving the common aim of the organization? Not much… Why expend massive resources to [maybe] detect mistakes vs. investment in mistake prevention instead? Simplify and streamline, using your existing technology to its full potential: this should be considered ‘plan A’.
Scenario: You might be worried that the operator does not enter the action contemporaneously into the batch record, therefore have a “verifier” e-sign alongside the operator – despite system audit trails capturing the time/date at which the action was recorded in the background, and could be used to re-create the GXP activity if any concern arose that could be linked back to non-contemporaneous record keeping. This verification makes little sense, unless we are talking about a lack of QA trust in operations staff due to previous mistakes. This breakdown in trust can easily happen when mistakes occur, so we must be careful and think objectively. Typically, the preventative action should not be to increase witnessing, but rather to GEMBA the workflow and identify opportunities to reduce mistakes through simplification and streamlining – taking full advantage of your existing technical solutions (in this case eBR): a much more effective CAPA vs. additional workload piled on operations…
In summary: treat witnessing/verification as a last resort. First try simplify and streamline using your existing technology as the “witness” and see how it works out. My bet is a notable example of continuous improvement…
Pete
November 10, 2025
Common Goals
Production is the economic engine of the plant. Quality is the patient representative (with ultimate authority) who acts as a coach, guiding production to achieve the highest quality product at the lowest price – maximizing both profit and reputation. The best coach is one who provides guidance and direction to achieve the common goal, in our case achieving this goal while working within the regulatory framework. Any activity introduced by the coach that is not aligned with the common goal nor required within the regulatory framework should be avoided. When approached objectively, the two departments should align more often than not. The problems arise when there is no clear understanding of risk acceptance within the Quality Unit - any risk identified during discussions is viewed as a regulatory noncompliance (gap), when in fact this is often not the case. QA is uncomfortable with risk, then attempts risk mitigation (which is not risk reduction) via additional procedural controls. Technical and engineering controls are typically the only the means for risk reduction, but are not always feasible. I would argue that in the majority of such instances, the best mitigation (when reduction is not possible) is a focus on simplification of the workflow rather than adding procedural steps that do little to achieve the common goal.
One massive source of quality problems (as we well know) come from mistakes - therefore we must focus on a reduction in mistakes through process excellence as “plan A” when risky (usually manual) operations are identified. Adding procedural controls (e.g., witnessing/verification) often increases the chances for mistakes (due to limited resources), inadvertently introducing quality problems despite good intentions.
To my QA friends & colleagues: before you roll out the next phase of your DI journey as an action item resulting from the new EU GMP framework – make sure your processes and mindset around risk mitigation are aligned with the principles of process excellence and a reduction in mistakes, otherwise the common goal may be difficult to achieve!
Pete
October 31st, 2025
Hybrid Systems
And Happy Halloween!
One controversial aspect of the new (draft) EU GMP Chapter 4 – which will also become a PIC/s Guidance once finalized, is the concept of the “hybrid system”, which is mentioned a total of 19 times in the document. I would like to provide my perspective on the hybrid system debate here, as it continues to be a source of significant regulatory confusion nearly 30 years after publication of FDA’s 21 CFR Part 11. Surprisingly, the question: “are hybrid systems acceptable in 2026?” is still a thing…
Part 1: To begin clarifying the murkiness, we must first define the concept of a “system”. FDA provided a clear outline of the “system” in their 2018 DI guidance, as follows:
“Computer or related systems can refer to computer hardware, software, peripheral devices, networks, cloud infrastructure, personnel, and associated documents (e.g., user manuals and standard operating procedures).”
A “system” is simply the sum total of arrangements that make up a GMP workflow, such as the offline testing of a sample for pH in the laboratory, which is a combination of software, hardware, personnel and documentation. This is likely also considered a “hybrid system”, as there is likely some paper documentation involved, and manual sample/instrument actions. Fully automated online pH measuring would not be considered a “hybrid system”.
A hybrid system is defined in the EU GMP as: “A combination of paper based and electronic means” to achieve a state of process/workflow validation. This is fully aligned with the previous FDA Guidance from 2018: nothing has changed here. A significant number of our GMP workflows are in fact “hybrid systems”. The number is reducing as automation accelerates, but they are unlikely to disappear anytime soon – hence the inclusion of the concept in the new regulation.
Part 2: Next, we must clarify the concept of “validation” – again there is significant confusion here. The regulators define validation as establishing by objective evidence that a process consistently produces its predetermined expectations. In 2026, this will mean providing the workflow data/process map, workflow risk assessment, and historical data demonstrating consistency. Note: historical data may not be available for new processes evaluated during pre-approval inspections. How much detail contained in the map/assessment and how much consistency (variability) are expected by the regulator, of course, depends on the intended use (criticality).
Part 3: Now let’s answer the question… Can the regulator do their job to protect public health if the data/metadata being submitted to demonstrate process consistency is in the form of paper – manually recorded by humans according to a training program and supplemented via good old fashioned trust? All historical data meets specifications, so nothing to see here… Is the “hybrid system” considered validated and ultimately acceptable if the site demonstrates consistent historical data meeting specifications outlined in the dossier, along with a process designed to include high risk paper-based controls? As usual, there is no right or wrong answer here… it depends.
Acceptability in 2026 really depends on what aspects of the hybrid system are paper-based. Most companies utilize a paper logbook to document unscheduled maintenance or troubleshooting, despite an extensive electronic audit trail: a “hybrid system”. This is due to the lack of interface between the production/lab and maintenance software programs. This facilitates traceability between the two systems, and will be needed to manage the risk of unauthorized system access until full digital convergence is achieved (not anytime soon).
On the other hand, some sites still utilize paper logbooks to supplement significant gaps in their production/laboratory assets, such as pH meters without the capability to save historical results (creating a printout as the “original record”). Defending workflow validation in this hybrid system will be nearly impossible in 2026, only maybe in the lowest criticality scenarios? Even the greatest control chart demonstrating historical consistency will be viewed as a waste of their valuable inspection time: “thanks for the information, feel free to submit it within 15-business-days.”
The key to understanding the acceptability of hybrid systems is understanding how the regulator views data risk – which is a prerequisite to demonstrating ALCOA+: a good explanation of which is provided in the new (draft) EU GMP Chapter 4. Specifically, the inclusion of the term “vulnerability” as an important dimension of risk. If a hazard related to accuracy or completeness of data (e.g. orphan data) is considered high due to lack of “appropriate controls” (significant vulnerability), the workflow will not be considered validated, despite beautiful PowerPoint presentations and 100% historical product acceptance. Again – feel free to respond in writing within 15-business-days. Don’t even begin to pretend you haven’t been warned.
Part 11 was published in the “late 1900’s”… c’mon now.
Pete
September 28th, 2025
The Bad Dream
Let’s Wake Up!
I’m sitting here on a flight en-route to EWR, and noticed a few birds flying by the window at ~5,000ft… this got me a bit freaked out and thinking about risk, so here we go!
As an industry, we must get over this unwarranted fear of risk. Risk is most often viewed as an unacceptable compliance issue, but in most cases this is simply not true. I cannot stress this enough. Processes involving humans performing manual actions will always be high risk, just like the best BBQ will always be in Texas. No one can argue with those two facts. Human involvement in our GXP workflows isn’t going anywhere anytime soon, it’s “industry standard”, so we must wake up from our dream-like-state and start to address our collective reality. Our workflows contain high, medium, and low risk steps, this is the reality - the same as crossing the street or driving a car inherently include various levels of risky hazards. You will agree with me that ignoring this reality while crossing the street is to your own peril. The exact same scenario in any given GXP workflow = ignore the reality of risk at your own (and unfortunately the patient’s) peril.
Management expects the righthand side of the assessment to be “all green”, by whatever means. This is an unfair expectation – a more realistic management expectation would be to produce the next batch on Mars. As a result, the assessment team struggles, argues, and ultimately formulates some form of electronic wallpaper to appease management and demonstrate “compliance”. Layers upon layers of procedural controls are dumped on front-line operations, and unsurprisingly operational deviations are not reduced… and FDA 483s continue to roll-in. I will [almost] always argue that traditional procedural controls such as additional paperwork achieve the opposite of their intention – and in fact increase risk [and deviations] through distraction and wasted resources.
I will argue in this blog that when a high-risk step is identified – the only means to reduce this reality is via reducing the “vulnerability” of the hazard [see Annex 11], generally through designing in technical/engineering controls. This takes time and investment, so in the meantime – focus your energy on employee engagement and empowerment instead. Additional layers of paperwork are viewed as “micromanagement” by production staff, and crush any cultural momentum. Don’t go down that path – it’s a dead end.
Check out section 10.2 of the new Annex 11:
“Where a routine work process requires that critical data be transferred from one system to another (e.g. from a laboratory instrument to a LIMS system), this should, where possible, be based on validated interfaces rather than on manual transcriptions. If critical data is transcribed manually, effective measures should be in place to ensure that this does not introduce any risk to data integrity.”
In this case, the regulator is not helping the situation… How can a site demonstrate that manual transcription (vs. a system interface) does not introduce any risk to data integrity? Impossible - so as result the old-habits will resurface. The knee-jerk reaction to this expectation of not introducing “any risk” to data integrity is going to be layers of extra paperwork, witnessing, and distraction.
Consider this instead: controlling risk through mutual respect. I trust and respect you to do your job so that our products are the best quality at the lowest price. If you deviate from the standard -that’s OK, bring it up and propose improvements. Management is listening! The reality is that the patient depends on the person to perform the manual transcription correctly (this is a fact), so instead of overcomplicating the process - set them up for success by removing distraction and permitting flow. Additional paperwork is a false sense of security and disrupts flow – again, we need to collectively wake up from this bad dream!
You might as well give it a try, because the status quo [obviously] does not work. History is an excellent teacher, so let’s start embracing the principles of Lean theory: especially the two main enablers: 1) respect for employees, and 2) continuous improvement. Start with (1), and (2) will follow organically. Here is my proposed roadmap:
1) Wake up from this bad dream,
2) Eliminate unnecessary procedural layers and focus on flow vs. “all green”,
3) Establish mutual respect between operations and management,
4) Enjoy the journey.
August 29, 2025
GXP & Lean
Are they compatible?
As many of you who study the principles of lean theory already know, the key strategy that forces continuous improvement and investing in employees is the one-piece flow cell (continuous manufacturing). Employing a one piece flow forces management to rely on continuous improvement and the ability of their employees to solve complex problems rapidly as they happen, due to no build-up of inventory. No inventory between process steps means a deviation in the workflow causes a paralysis of the line and idle downstream workers. It is definitely a risk and will most certainly cause short-term pain, but the long-term payoffs are immense: higher quality products, cost savings, better employee retention, and facilitating a [real] great place to work. No need to add any references or case studies here, this has been proven over and over again since the 1950’s.
The issue I would like to address in this blog is that most of us working within the GXP world do not deploy one piece flow cells (this can also be services/etc., it does not need to be a drug component/substance/product). In fact, a one piece flow may not always make sense in our GXP universe, due to a variety of complex factors. As a result, however, we are not forced to focus on the two key pillars of lean:
Continuous Improvement
Employee Engagement and Empowerment
As a result, we need to find another ‘forcing function’ that directs management to treat the two key pillars above as necessary for survival. The regulators are well aware of this reality, many of which are masters of lean theory, and have as a result tried their best to update regulation (Annex 11) and guidance (QMM) to ‘force’ us to embrace the components of lean where we can. Lean processes are not an ‘all-or-nothing’ endeavor. We can extract the strategies (pull vs. push) where we can, and just do the best we can with what we have.
Data Governance, written into the new Annex 11, EU GMP Chapter 4, and ICH E6(R3), is a theory that ‘forces’ us to embrace a “risk-based approach” to GXP workflows. When the site is able to create a mental map of a “risk-based approach” via data governance and lean theory, they will find serious overlap. In fact, I would argue there is no principle of lean that cannot be deployed within a “risk-based approach”. You may never be lucky enough to work within a truly lean organization deploying continuous flow cells.
That’s OK, if you instead replace this (continuous processes) with the common aim/key corporate strategy of data governance, which if understood at its core (join us in an upcoming workshop to explore the concept in depth), will ‘force’ management to embrace the two pillars listed above as necessary for survival.
August 9, 2025
Why Annex/Part 11
Why the core GXP regulations are not enough
There is much chatter on LinkedIn and within the Pharma Community about the revisions to Annex 11, which will automatically also become a harmonized worldwide PIC/s Guidance following the final revisions. Regardless of what you think about the content of the newly proposed regulation, in this blog I would like to address the “why” behind the need for specific regulation for GXP data collected/reviewed/etc. within electronic systems. Shouldn’t the EU GMP chapter 4 (Documentation) or FDA’s GCP found in the 320’s be sufficient to provide assurance of product quality and patient safety? Why do we need extra regulations that are so specific…?
My favorite quotes for defending any regulation (at least in the US) are found the “preambles” published within the Federal Register – an incredibly boring but yet still somehow interesting ‘magazine’. Random side note: do kids these days even know what a ‘magazine’ looks like? One of my all-time-favs is the Part 11 Preamble, published in 1997 (notably the same year that DVDs launched in the USA, remember those??). So, without further ado, enjoy the read:
Federal Register / Vol. 62, No. 54 / Thursday, March 20, 1997
“Absent effective controls, it is very easy to falsify electronic records to render them indistinguishable from original, true records. The traditional paper record, in comparison, is generally a durable unitized representation that is fixed in time and space. Information is recorded directly in a manner that does not require an intermediate means of interpretation. When an incorrect entry is made, the customary method of correcting FDA related records is to cross out the original entry in a manner that does not obscure the prior data. Although paper records may be falsified, it is relatively difficult (in comparison to falsification of electronic records) to do so in a nondetectable manner. In the case of paper records that have been falsified, a body of evidence exists that can help prove that the records had been changed; comparable methods to detect falsification of electronic records have yet to be fully developed.”
August 5, 2025
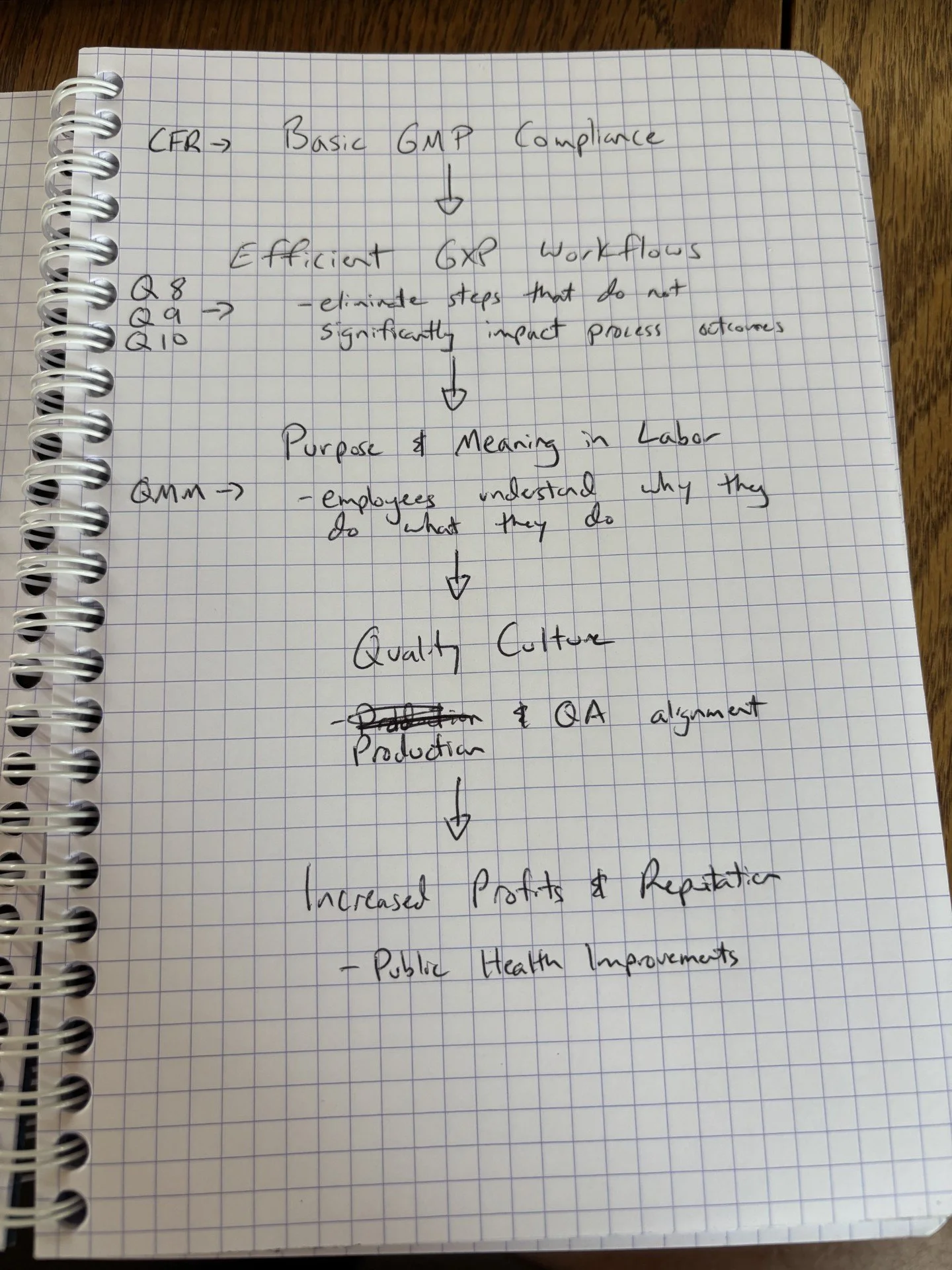
Quality & the Business
Quality Management Initiatives in the Pharmaceutical Industry: An Economic Perspective
CDER has just released, with very little fanfare, the next publication in their Quality Management Maturity (QMM) series, titled “Quality Management Initiatives in the Pharmaceutical Industry: An Economic Perspective” which is a pretty big deal! This is not considered a ‘Guidance for Industry’, but rather a ‘Whitepaper’ in line with previous QMM publications and others such as Drug Shortages. The primary objective of QMM has and will remain reducing shortages, attempting to argue the business case for Quality and healthy market competition. Whitepapers are typically released to address ongoing public health challenges with incentives vs. outlining minimum expectations, as in traditional Guidance Documents. This one appears to have been largely generated by an AI assistant – probably Elsa, as there are likely terabytes of data on the internet about Quality Management and the business case for Quality (just not necessarily from our industry, unfortunately…).
In this case, the incentives presented by CDER are clear: if you focus on the ‘old school’ principles of Quality Management, financial benefits come naturally. Quality and Profit do not need to be opposing forces. ICH Q9: Quality Risk Management (QRM), was published some 15+ years ago and is a model summary of ‘old school quality’, but still (despite recent revisions) remains bare bones and does not include any practical framework to apply its concepts. Perhaps this Whitepaper is an attempt to provide some structure for how to apply QRM in GXP, as the “Lean Six Sigma” manufacturing theory is mentioned multiple times. Lean Six Sigma is a very specific framework for reducing process variation, and can be very effective when applied to largely automated processes or assembly lines (e.g., FMEA is a primary tool, which results in disaster when used without supporting data sets). Lean, on the other hand, is based on more qualitative tools, and is better equipped to handle manual and hybrid processes, such as those found in abundance in our industry.
This lack of structure within Q9, which is expertly written to address both automated, hybrid and manual processes, is likely the reason many companies have left it on the shelf to accumulate dust, or treated it more as a checkbox compliance activity rather than a guide to achieve excellence in manufacturing. Most GXP management has nightmares of acknowledging GXP process hazards, preferring instead to keep risk in the shadows and instead blame the worker (human error) for any quality lapse. This is absolutely 100% prohibited in Lean theory, as problems must first be attributed to the process design before any human error can be considered.
I have personally not recommended any one Quality theory to adhere to, preferring the flexibility that comes with simple tools and critical thinking – but maybe it’s time to adopt a more structured and formal approach to QRM? Maybe a structured approach, with study materials and certifications, will finally push us in the right direction? I remain skeptical that this approach will work on a large scale within the GXP world (as the tools are too formal). I think the basic ‘old school’ 1950’s Lean principles, combined with Q9, may provide enough structure, without the “six sigma” addition.
The concepts of Data Governance, outlined in the new PIC/s Guide and associated Annex 11 regulation, provide this middle-ground structure vs. flexibility answer we need. Make sure to join us in an upcoming workshop as we discuss the structure and theory necessary to get started, with the goal of long-term compliance/quality and profitability!
Pete
August 1, 2025
Golden Batch
really?
In the cafeteria during a recent on-site visit, I observed staff indulging in a wonderful buffet including a full spread of appetizers, mains and deserts… along with some nice drinks. Of course I had to inquire: what’s this all about? The answer was that the site had recently achieved a “Golden Batch”. I congratulated the team on a job well done, but the GXP Quality side of my brain had some serious lingering concerns, which I chose to keep to myself, obviously… Let’s get into it here.
The idea of a Golden Batch is a popular concept within the lean manufacturing camp (I am permanently camped out here…), and can be roughly defined as ‘the ideal production run where each parameter that may be susceptible to variability such as materials, temperature, pressure, mixing speed, time, etc., meet their ideal values within the specification range to produce the highest quality product with the lowest waste and therefore lowest cost.’
Problem #1: Most of us do not know the ideal range within our specifications that achieve the goal of highest quality at lowest price…
Problem #2: The definition is silent with regard to deviations. In fact, a Golden Batch in lean theory can still experience multiple deviations during the production run. The Golden Batch is all about measuring process/parameter variability (it is solely process parameter data-driven)! Unfortunately, however, for whatever reason we in GXP have also tagged on the idea of “zero deviations” (this makes me cringe), which is the exact opposite of the lean mindset. This is added goal is excess overweight baggage, and will incur significant penalties! To be fair, in theory, this is not a bad endeavor, but it requires a very, very high level of QMM to realistically achieve its goals within the highly regulated GXP manufacturing space. Without a mature Quality Mindset, the “Gold” in Golden will be as elusive to your organization as a leprechaun’s treasure at the end of the rainbow (for reference: it’s not real).
Why? Because in my experience most GXP manufacturing sites still treat deviation investigations, for example, as a failure (negative metric) instead of an opportunity for growth. Deviations as a key ingredient for continuous improvement and growth is a foundational principle for lean manufacturing sites. In their perspective, it would be impossible to achieve a Golden Batch without a mature investigations process… This perception of a negative metric within the GXP community, combined with the rewards that come with the Golden Batch, are a recipe for disaster in sites that have not yet set foot on FDA’s QMM ladder. These sites may skip the hard part (continuous improvement over months/years) that is an absolute prerequisite to achieve the Golden Batch. Anyone can achieve a Golden Batch (on paper), but does it really meet the spirit within the lean mindset?
Pete
July 20, 2025
Quality Culture
abstract or tangible?
Today, culture is on my mind. We hear much talk on the subject, but I personally dislike the way we often use the term in the abstract when applied to GXP organizations. Culture does not have to be an abstract concept; simply unable to be measured. I find senior leadership may at times use culture as a distraction by treating it as something that is felt rather than realized. Treating culture as abstract feeling dilutes its significance and can be used an excuse not to focus on tangible results that may actually realize the defining nature of culture: summarized as ‘purpose and meaning in labor’. When we humans find purpose and meaning in work, only then can a common aim among various departments be realized – typically safe and effective medicines. We achieve purpose and meaning in labor by ensuring any action required by an operator or analyst has a reason behind it, and that reason is because it in some way impacts a patient.
Developing SOPs that ensure tasks are meaningful is not easy. The easier route is volume - simply do everything, which will inevitably also include the meaningful tasks. Inspections will come and go without much disruption, but so will valuable employees… For these organizations that focus on volume rather than meaning, culture must be spoken of in the abstract, because it will never be realized. Volume is the enemy of quality culture… Luckily, a clear roadmap to eliminate unnecessary tasks has been published by the regulators years ago!
A simple and tangible roadmap to culture is sketched out below: it’s not too difficult – so get onboard!
Pete
June 27, 2025
Sounding the Alarm
AI Chatbots and GXP Compliance
It’s 7am here in Utah, and already the sun is bearing down - time to get some thoughts on paper before the heat truly sets in!
In my recent Investigations & CAPA workshop, the question was posed something to the tune of: “is it OK that we use our enterprise chatbot for assisting with the drafting of deviations text?”. “Sure”, I replied – “AI assistants can assist with deviation management in a variety of ways, from historical trend analysis to root cause analysis, among others”. As this particular workflow is meant to primarily comply with 21 CFR Part 211.192 [investigations into unexplained discrepancies], I obviously had to follow-up with the following statement: “what documentation might you have available to the regulator to demonstrate a validated workflow?” Note deliberate wordsmithing here, I am referencing Process Validation Guidance, as the introduction of an AI assistant to meet a GMP predicate rule certainly needs controls to ensure a “high degree of assurance” that the workflow will produce an outcome commensurate with its risk to product/patient.
The PIC/s Guide for Data Management gives us an excellent roadmap here in its outline of the principles of Process/Data Governance [design – operation – monitoring]. If I was the regulator, I would simply ask the site to demonstrate each of the 3 governance principles have been met and the site has a clear understanding of the validated workflow. I would already have ‘targets’ in mind that must be answered during the inspection, here are just two of several:
Inaccurate Information: inaccuracy and hallucination is a well-known risk associated with the use of chatbots: making up information that is not true. Anyone who has used Chatbots knows this happens on a regular basis (I have to admit that I recently purchased an incorrect bike tube based on wrong information that the chatbot proposed as a statement of material fact. It was incorrect and I am now stuck with a useless tube, I should have verified with the user manual or Reddit but that takes time…). The root cause of this risk is difficult to pinpoint and even more difficult to control.
Inspection Strategy: ask the QA associate if all the facts included in the deviation text are statements of material fact. As they may have been drafted by the chatbot, did they perform interviews with staff to confirm the statements and conclusions made by the chatbot? Did the associate account for any recent process changes, as the model is proposing details based on an averaging/weighting of historical [and potentially outdated] knowledge (is unaware of the larger quality system, unlike the human). This is unlikely, because the convenience of using a chatbot makes assuming the accuracy of the model output too easy [going to interview staff takes time, for example]. Here I start to lose confidence in the ALCOA of the deviations data (specifically accuracy). Don’t blame the QA associate for this, it is simply human nature to take the path of least resistance, blame the head of QA or CDO for failing to understand the principles of ICH Q9… Assuming the accuracy of chatbot outputs is a disaster in the making – in my opinion it is only a matter of time until the recalls and regulatory actions start. Inaccurate data in deviations has always been a risk factor considered during inspection, but was not a main concern as it was very difficult to cite on a 483. In the future, it becomes easy if clear instructions on how to control the risk from inaccuracy and hallucination is not clearly identified (design stage), controlled (operations stage) and regulatory evaluated (monitoring stage).
Bias: As more repetitive information is fed into the data set and the model is automatically and/or manually fine-tuned, an echo chamber of repeating information is a risk factor that will occur if not governed. This is one manifestation of bias, among others. This risk is closely related to inaccuracy/hallucination, but it is important to break it out as a separate hazard as it must be controlled differently.
Inspection Strategy: request a list of root cause conclusions, and look for repeats. Well designed and controlled AI models are decent critical thinkers, but this takes expertise and risk management from the admin to the operations level. Without this expertise and active control strategy, bias is almost certain to manifest itself in repeated information/conclusions. Has the staff considered all potential relevant contributing factors prior to signing off (per the SOP), or was the model output assumed to be correct (or the SOP is silent). The PIC/s guide for inspecting a risk management program (a little known but excellent guidance) proposes 3 main observations in the universe of risk management, one of which is termed “unfair assumptions”. Here is where this becomes easy to cite.
Historically, these two bullet points have been cited countless times in FDA 483’s, obviously. The difference is that the scope of the observation is limited (2-3 deviations, or a small cluster considered deficient). The risk to the patient has always been present, but the diversity of humans in QA has mitigated the risk via limitation of scope. In the world of chatbots, the scope may be considered “all”, todo, tous, alle… Yes, the human is still in line, but can they still be considered an adequate risk control measure? I think it is time to sound the alarm, as there are currently an absence of ‘effective control measures’ in place and the entire deviations program is vulnerable to collapse during an external inspection. The ungoverned use of chatbots is reckless, and ultimately unfair to the patients we serve. We can do better.
Pete
May 26th, 2025
Paradox of Choice
less is more
When executing a risk assessment, the scales/standards used to define the ‘severity’ and ‘vulnerability’ values for any given hazard [to determine the risk] is a key starting point. Get the scales wrong, and the whole effort is likely for nothing, causing your organization to lose confidence in the theory of a ‘risk based approach’ being better than conventional decision-making after several regulatory (or internal) observations on the trot. The organization will likely revert back to the practice of generational pass-down of knowledge via storytelling, much like we [humanity] have done for millennia. Entertaining, but incredibly inefficient. For example: ‘we did it like this before, and never received an observation’… sound familiar? Cool story bro! Ugh, please get me on the first flight back to Austin.
There are several key points to understand when designing the assessment scoring scales. However, in this blog entry we will cover just one key design element: simplicity. As humans, we are prone to the cognitive challenge defined as the “Paradox of Choice”. How many of you have struggled to decide on what to eat at the Cheesecake Factory? As of today, they have over 250 potential choices on the menu – which one is good, which one is the best… what should I order? Impossible to determine.
This decision-making problem is defined as the Paradox of Choice. Once a human is presented with a large number of potential choices, two things happen:
1. Mental exhaustion leading to paralysis
2. Dissatisfaction with the end result (as a result of second-guessing)
Maybe this is why I avoid the Cheesecake Factory like the plague? Probably not only for that reason, but I digress…
Within a highly regulated environment, where we deal with life/death decisions, choosing the wrong option is scary, hence we strive to find the “right answer”. Unfortunately, however, there are no right/wrong answers in assessing risk, as determining future (or past) performance of a machine or human is an impossible task – all we can do is get close to the right answer (hence my 100% belief in qualitative vs. quantitative assessments). I consistently come across scoring scales that have 5 or more potential options for both severity and vulnerability (vs. the core three: high/medium/low). It appears that these folks have fallen into the fallacy of “more is better”. Somehow more scientific, more compliant? Wrong, that’s old school. In this case – less is better. In order for the critical thinking side of your brain to kick into high gear, it needs 1) energy, and 2) confidence. When presented with too many choices, it shuts down and hibernates until recovered.
So what can we do about it, Pete? I argue in this blog that three things will happen as a result of simplification of the scoring scales (high, medium, low):
1. More participation in the QRM program due to less mental exhaustion
2. More confidence in data governance outcomes due to less second-guessing and wondering if the wrong choice was made (…should I have ordered the tacos…?)
3. Easy inspections – people know what they do, and [more importantly] why they do it.
Pete
May 22nd, 2025
The 80/20 Rule
as it applies to QRM…
Initiating a data governance project at any given site around the world has to start with a problem statement. Without this, the project will likely die a slow and painful death because no one is really sure what was the project was all about in the first place… Folks will likely think (or even verbalize): “don’t we already have a data integrity program in place”? The answer is likely yes, it just isn’t very good. In reality, no one is happy with the level of audit trail review, data reconciliation, or witnessing burdens that are placed on staff members. In my experience, the problem statement is [nearly] universal: the current DI program is not truly “risk based” and therefore likely failing regulatory expectations: hence the continuous stream of 483s citing deficiencies to 21 CFR Part 211.68. Semi-structured DI checklists simply fail to do the job we ask of them (it’s not their fault, don’t blame the checklist!) due to their failure to connect with the process “workflow” (see FDA DI Guidance Q3). On this blog page, I have already written about the two tools used to establish data governance: 1) data/process mapping and 2) qualitative risk assessments using the principles of a) severity and b) vulnerability. In our data governance workshops, we now use AI tools to assist with rapid generation of data/process maps, which is a game changer… I am not going to address this point in this blog entry, but rather the second, more difficult tool: qualitative risk assessments. AI can assist here as well, although the human is much more integrated and critical the process outcome.
The purpose of this blog entry is to address the main roadblock to achieving rapid/agile risk assessments: the problem of when the risk assessment complete? If you were tasked with performing a risk assessment for driving to the grocery store, you could identify, evaluate and attempt to control an unlimited number of hazards… For example, the hazard: “large hailstorm forms and shatters windshield”. You could, in theory, evaluate the risk, and put in controls in place such as install bullet-proof glass. This would reduce the risk of this hazard causing a failure to the process. The list of hazards is in reality to infinity and beyond, however, this would cause what we call “perfection paralysis”, and your refrigerator would quickly run out of goods (unless you live in a city with a delivery service).
As a result of this risk-reality, we as humans often follow the 80/20 rule, including within the science of project management. For example, 80% of a project’s benefits are likely achieved via 20% of the existing efforts. The remaining 80% of effort is only achieving 20% of the project’s benefits. In the GXP realm, this is also likely to be true! Most of our patient safety/quality assurance is achieved via just a few actions performed by operations/QA staff. In the DI world, this is simply those actions that ensure the 1) accuracy and 2) completeness of data.
So how can we take this fundamental and well established principle of project management and put it to use in our data governance program? The answer is clear, focus on the big stuff, and don’t sweat the small stuff (sorry for the cliche but it is just too appropriate!). Remember that the majority of your risk is covered by evaluating just a few process hazards, and that is sufficient. If you have a gap in the big stuff (e.g. lack of access controls), focus your limited resources on fixing those using innovative and possibly non-traditional GXP technology, instead of wasting efforts on an encyclopedia-style risk assessment that burns the midnight oil and leaves everyone exhausted. There is no gas in the tank to fix - it was all expended assessing… If you miss something small, don’t worry - trending, deviations, or CPV will catch it, and it can be addressed then and there - therein lies the beauty of a lifecycle approach to validation. Remember that the vast majority of risk exists within just a few hazards, and you are not likely to miss those. The patient expects medicines that are safe [obviously] but also affordable. Keep the 80/20 rule in mind, and your organization will thrive. Give yourself a timeframe to complete the risk assessment (my advice = 4 hours maximum) - and stick to it.
As a Texan, I am [obviously] a country music fan. If you need a little motivation here, just listen to the incredible song by Kevin S. Wilson - Don't Sweat The Small Stuff. Listen as a group before you start the risk assessment, you will crush it!
Pete
April 25th, 2025
Critical Thinking
what it is not…
It’s starting to heat up here in Austin, hence spending the afternoon indoors… thought I might get to some writing! Lately I have been doing some research into the concept of “critical thinking” – as I would like for it to have actual meaning in my workshops and not be automatically dismissed as generic or cliché. Treating critical thinking as a “buzz word” would be tragedy, as the concept is essential for success in the new world of automation and big data management. The definition for critical thinking varies widely between publications, it seems there is no universal definition nor even a largely harmonized view. Here is a definition that I think sums up the compilation of viewpoints I have reviewed:
“Considering both what you know and what you don’t know prior to decision-making, with the goal of producing an objective outcome”
The word “critical” comes from the Greek “kritikos” – meaning something to the tune of “to discern”. This is not to be confused with the act of being critical of an idea or proposal… this is much different! In my experience, this is one of the major roadblocks in our industry, the confusion of being critical vs. being discerning… During cross-functional meetings, we often find problem solving difficult because we lack a structured process for discerning the issue at hand, and as a result the project is delayed or just plain cancelled as a consensus cannot be reached as we have no means to deal with critical viewpoints/roadblocks… (hence ancient pH meters floating around out there lacking any sort of data management, the use of flat files, paper-on-glass, annotations… OK I will stop there). The roadblock might be legit, but it must be backed up with objectivity, or it will be taken as an opinion and the project begins to deteriorate quickly.
My recommendation, if your goal is to be a problem solver rather than be seen as a problem creator is to focus on developing a structured approach to discerning the problem at hand, considering what you know and what you don’t know prior to taking any position or especially prior to throwing up any roadblocks. Can you make an objective contribution considering subjectivity in the equation? Yep. ICH Q9 is always there as an excellent and free resource, and of course comes with the regulatory seal of approval if the fabulous four Q9 concepts (criticality, risk, severity, probability) CRSP [pronounced “crisp”] are utilized according to the guidance - or for an even simpler approach, a simple list with two columns works like magic.
Pete
April 8th, 2025
Common Sense Quality
an epic adventure
Waiting for a flight here in Colorado, and finally have some time to sit down and write! I spent the weekend snowboarding, and had quite a bit of time to think and reflect while on the lifts up to 12,000ft. 2ft of fresh powder was a nice added benefit!
Growing up in rural Oregon, we really only had one mountain that was doable for a day trip: Hoodoo. It’s a small family-run “resort” with a few old-style lifts and not much else going on. Because of its small size, to achieve the sense of adventure that we craved as kids, we had to spend time exploring the out-of-bounds backcountry. We would take the lifts up and then disappear, spending hours out there finding new runs, building jumps, and hiking around in the snow. Over time, I learned that to be a decent backcountry snowboarder, risk management is critical. Split-second left or right decisions will make or break (literally) your day.
Reflecting back on these early memories this week, I realized that the best choice (right or left) while ripping down through the trees was always the path of least resistance. You could go the harder route, but you would often end up getting buried in a tree well and calling your buddies to help dig you out. Initially it seems like a better adventure, but turns out to be no fun for anyone. As I grew older, I learned that the harder routes rarely paid off in our quest for adventure. Significant delays, loss of energy, and overall less enjoyment/adventure (not to mention possible injury).
I feel that we in the GXP world are still learning these lessons. We often take the path of greater resistance, but instead of seeking adventure we do it in search of compliance. It has been my experience, however, that compliance is most likely achieved when we take the path of least resistance. In 2025, GXP compliance can most accurately be summarized by extracting a common thread from FDA Warning Letters: “vigilant operations management oversight”. There is no way to vigilantly monitor complex and subjective workflows… impossible. Many folks agree with me, in theory, but have trouble making the jump and implementing lean GXP workflows, likely do to fear. Overcoming this fear can only be achieved via practice, just like back-country snowboarding. Start small, run a few pilots… Demonstrate the patient and business benefits (they will fully align if the proper resources are available), and start a cultural shift to the path of least resistance. In our governance workshops, we use a phrase to summarize the goal: “Common Sense Quality”.
With practice and determination, you will find that common sense quality relies on developing GXP workflows that choose the path of least resistance (Qualification/SOPs/training/etc…). Why are operators required to “train” on 14 random SOP’s per week? This is an example of the opposite of common sense quality, it is a company lost in the woods. These operators will likely get stuck in the trees and require rescuing! On the other hand, vigilant operations management oversight of the training program will result in assigning only the SOPs relevant to their workload, and supplement others via optional modules and/or periodic all-hands where site-wide trends are addressed.
Don’t be afraid – explore carving the path of least resistance and common sense quality, the adventure and rewards are epic!
March 31, 2025
Dismantling Validation
for a real digital transformation
Before a meaningful digital transformation can occur within your organization, a full dismantling and rebuild of the traditional ‘validation’ framework is required. As the next generation of employees join our industry, they will likely be dumbfounded by the lack of digitalization and common-sense approaches to quality, and may resort to parallel solutions (and unanticipated risks) if we do not adapt. We must go further than a simple mindset shift – such as “we now take a CSA approach”, which is often a half-hearted effort that will likely result in confusion rather than solution. We need to go all in.
Steps for success:
Breakdown ‘validation’ into its individual components (hardware, software, personnel, documentation)
New definitions (e.g., ‘qualification’) and work streams (e.g., Quality Intelligence) are needed
New risk-management tools are [definitely] required (e.g., qualitative) - no quantitative tools allowed, without compromise
Run a pilot, followed by presentation of the business and GXP perspectives to senior leadership
In my experience, you will find that if your organization is equipped with the mindset and appropriate toolbox, cost and quality have a more nuanced relationship than was historically thought to be true…. Does higher quality require bigger budgets? Maybe not.
To realize that opportunity, however, your origination must approach this issue more like a re-build than a re-model, for those of you who have ever been a home owner…
A simple visual representation with three product streams is outlined below, and for a deep dive, join us in Austin for a week long re-building journey:
February 15, 2025
Risk Approximation
As close to the target as possible
It’s a rainy day here in Dublin, so might as well write a blog entry: so they say…
Yesterday in the car on the cross-country drive I was listening to a podcast on personal finance, and one quote by the guest Ramit Sethi hit me with a significant force. Mr. Sethi stated that a person’s attitude about money has little correlation with the amount in their account. Rather, it is based on a multitude of life experiences starting from a very young age. Interesting.
As a consultant working primarily in the area of data and risk management, I find this statement to be a near perfect description of what we find in our world as well: a site’s perception of process/data risk has little correlation with the actual risk within the process. Just like finance, it is rather based on a lifetime of experiences such as inspections, trainings, pervious company directives, etc. We might call these biases. As an industry, we need to fix this discrepancy, and it starts with establishing clear standards for the factors of risk assessment, as an attempt to replace bias with science. For example, what is the definition of a medium severity score, or a low vulnerability score? Is it vague and therefore based on the assessor’s biases? If yes; not a recipe for success.
Try establishing standards that are as objective as possible. For example, is a technical or engineering control available that can prevent a hazard from occurring? If yes, that is assigned a low vulnerability score. If not, the assessor may not use other factors to achieve the same conclusion of “low”. Nope, no chance. Gone are the days of “faking it until we make it” in QRM; clear standards make this impossible. Faking a risk conclusion is no different than bending the laws of physics… good luck.
A risk assessment is never going to be a direct evaluation of patient risk, it will always be an indirect approximation. Our job is to get this indirect approximation to be as close to the target as possible.
Join us in Austin or Dublin at the Governance Workshop as we work through what good standards look like, and how to achieve both self and organizational transformation. Hope to see you there!
Pete
February 2, 2025
“all sources of variability”
Key to “thorough investigations”
FDA recently published a GMP Warning Letter issued January 15th, mainly focused on “failure to investigate all critical deviations”, among other issues. Warning Letters such as this give us an insight into current regulatory expectations for compliance with 211.192, which are important, as there is little guidance available regarding the expectation that manufacturing events be “thoroughly investigated”. What constitutes a “thorough” investigation in 2025? What does a good root cause analysis look like, and what tools should we use to determine product impact?
This warning letter gives us some strong insight. Although the remediation instructions for the company are not necessarily new, they are an excellent reminder, considering the “C” in CGMP always moves forward - never backward. Here are some takeaways to keep in mind, and may be useful to your organization as an internal maturity check:
Understanding process variability is key to demonstrating root causes.
The letter recommends that for issues where no determinate root cause has been identified during the failure investigation, the company perform a “thorough” review of potential production factors that could have led to the failure. This is no easy task, considering a review of documentation (e.g., batch record) is unlikely to identify an obvious cause. Once the low hanging fruit has all been picked, the next step requires identifying potential causes via “scientific” rationale (the hard part). Listing potential causes here based on opinion or best efforts will be considered insufficient, as it is not scientific. The scientific part here means speaking the language of QRM, but without an understanding of process risk and a knowledge management program to turn to, the team performing the investigation is stuck with nowhere to turn, the hard part is actually impossible!
Finding the root cause and therefore the product impact in these situations is unlikely to happen. The best the team can do is to:
Point to the most likely sources of the failure (via reference to a documented process & data risk assessment)
Evaluate worst case (patient) scenarios for each element
Make the conclusion, being transparent that this is not objective, but as objective as possible considering the circumstances and residual patient risk. Every decision to close an investigation involves some level of subjectivity. That’s OK, the regulators are simply requesting that the decision be as objective as possible, following good scientific practices
Decisions should be “data driven”.
Understanding “all sources of variability” via a process-level granular risk assessment and subsequent targeted data monitoring program (we might call this CPV) greatly enhances the ability of the team to increase the level of objectivity in the final impact statement, not to mention result in meaningful CAPAs, rather than the traditional expansion of work instructions/training and more best efforts at the floor level.
The letter goes on to describe some elements of this transformation, many of which have been outlined in this blog (hence the statement above that this is not necessarily anything new).
In summary, it might be wise to reflect on your current organization’s maturity regarding these two points. Are your investigation teams set up for success in 2025? Do they have a knowledge management program (see ICH Q8/9/10) to turn to when difficult situations arise? Solving the difficult problems requires a quality system transformation, this is clearly evident in the letter. Although you may not be able to transform an entire organization, can you transform your department or division? Start small.
Map out your workflow and identify “all sources of variability”.
Perform a risk qualitative risk assessment using the concepts of severity and vulnerability.
Trace them back to your current process.
Do you have the data you need to monitor variability, if yes - create a dashboard
Don’t get hung up with perfection, just do what you can do within your department, and before you know it you will have a division that serves as the model for the organization! If you are looking for a solution that will achieve full objectivity, I’m afraid I have bad news… Just do the best you can with what you have, and let the future be the judge.
Pete
January 12, 2025
Draft Guidance
211.110 (Process Validation & Control)
Like many in industry, I was somewhat surprised by the publication of the FDA draft guidance earlier this month, titled “Considerations for Complying With 21 CFR 211.110”. My first thoughts were publication due to the need to clarify the phrase “vigilant operations management oversight”, which is often cited in modern Warning Letters when sites lose focus on quality operations. As I read through the document, which is quite short, I found this may hold some truth, but really I found what appears to be a summary of already existing guidance (which are each listed at the conclusion of the document…). I had to read the document a second time to determine if there is any new guidance and/or expectations included. After a second reading, here are some of the key takeaways, in my opinion, although I could argue that these have been around for some time already:
In-process monitoring/sampling should not be considered solely a compliance activity based on traditional manufacturing strategies. The strategy for any in-process sampling/monitoring should be based on a risk assessment and process knowledge. This has been built into the regulation since forever via the use of the phrase “where appropriate”, which is included in both 110(a) and 110(b), we just haven’t been very good at demonstrating what is appropriate. Each process has its own unique characteristics, which should be identified and evaluated according to QRM principles, and not just based on the strategies used since the late 1900’s. Here we find some language largely drawn from the existing data integrity guideline: “Manufacturers must maintain the process in a state of control over the life of the process to ensure drug product quality, even as materials, equipment, production environment, personnel, and manufacturing procedures change”.
This is largely aligned with the components of a validated workflow outlined in the existing FDA DI guidance: “hardware, software, personnel, documentation”. Basically, if you are going to sample, monitor, or both, make sure your rationale for why you do what you do is based on risks that exist within the workflows, in addition to other factors such as chemistry/etc.
The guideline clarifies the definition of a “significant phase”, and follows up the discussion with an example of a process where only minor adjustments are permitted. If effective controls over changes to parameters are achieved via technical means (e.g. access controls), there may not be a need to implement extensive Quality Unit oversight. A simple review of a batch summary may suffice.
I very much like the inclusion of this example, as it backs up the existing guidance provided in the PIC/s guide for Data Governance, and provides a practical example of “review by exception” or a “risk-based approach” to QA oversight. Basically, don’t waste resources on extensive monitoring and oversight if you have invested in process understanding and digital solutions. This action would not be “significant”!
Use innovative means for process monitoring. Options include traditional offline testing (expensive and error-prone), in-process monitoring, or a combination of in-process monitoring and mathematical modeling. The latter is better, if possible!
Advanced Manufacturing is not quite ready to go live, unfortunately. In the final section of the guide, we find additional guidance largely in line with Q8, QRM and PAT existing guidance. Advanced manufacturing is no doubt the future, so what is the delay? It appears that proposals submitted thus far have lacked scientific rationale. For example, a lack of a QRM strategy for an “unplanned disturbance” that may occur during the process. Without a thorough QRM plan established where extensive hazards (planned and unplanned) are evaluated, it is unlikely that we as an industry can move forward in this space. It seems we need more work in this area.
In summary, I see FDA publishing a brief reminder that QRM is not optional, regardless of whether the dosage form has been around forever (e.g. rapid release tablets), and a statement on the current state of affairs regarding future technologies for process control (it’s not ready to go live). I see this publication largely in response to the record number of drug shortages being experienced in the past year… The root causes largely being attributed to “manufacturing and quality issues”. Basically, we need to get better at what we should have been doing since forever = QRM.
Pete
December 1, 2024
Doc Control: when is enough, enough?
While browsing recent FDA 483’s within the Redica database, I came across a 483 (issued September 27, 2024) that may give us an insight regarding regulatory expectations for the management of in-process CGMP documentation that will eventually be used (e.g., uploaded to an eQMS) to support an investigation initiated under 211.192. For example, the use of MS Word, Excel, or even printed blank paper forms to document steps taken during an incident, investigation, OOX, etc… Here is the text, which was cited under 211.68(b):
“General Format documents not controlled or reconciled. These forms can be used in part for DEV/CAPA investigations, assessment/evaluation of CAPAs, and as a form for attaching data printouts.”
In this case, there were no controls implemented for “General Format” forms, meaning they can be easily replaced without a trace. In most cases, firms use Word for such activities, which presents its own challenge! The use of any software to support an investigation (a predicate rule!) would certainly need to meet the expectations outlined in 21 CFR Part 11, just like paper forms must meet doc control expectations, however, we have so far not considered this to be relevant. So where do we currently stand with regard to software and investigations? I’m afraid this is unacknowledged risk…
Many firms use Word/etc. to document the steps taken during the investigation, including a description of the event, evaluation of scope, root cause analysis, product impact, and CAPA. All of this is done without any controls! This data, which in many cases directly impacts a patient if incorrect or inaccurate, is essentially ungoverned. In fact, most firms don’t even mention the use of Word within their investigation SOPs/work instructions!
If this would be cited on an FDA 483, the investigator would need to answer the “so what” question. So here we go, I might write it as follows, cited under 211.68(b):
Appropriate controls are not exercised over computers or related systems to assure that changes in master production and control records are instituted by authorized personnel. Specifically,
Your firm uses MS Word to document CGMP original data collected during the OOX, deviation, incident, and complaint investigation processes. There are no written procedures established to describe the use of MS Word during the investigation process. Additionally, no risk assessment has been completed to identify any residual risk in the current unofficial workflow regarding the accuracy and completeness of CGMP data and/or metadata.
For example, during my review of the laptop assigned to your QA Associate, I noted at least 6 ongoing deviation investigations stored within the “Deviations” shared folder that were partially completed. No audit trail is available to evaluate the creation, modification and deletion of this data.
As a result, the accuracy and completeness of data collected during the investigations process and ultimately uploaded to your eQMS cannot be verified.
Have details collected during the initial scope evaluation been removed or altered to fit the product impact assessment? This may be done with the best of intentions, however, it may have unintended consequences. In my opinion, this is unacceptable residual risk. Even if we were operating in a largely unregulated environment, such as the manufacture of smartphones, this would be bad for business. Senior management should be hungry for the real and unfiltered metrics/state of quality, which originate at the front line but are often diluted and/or biased as they move up the chain to the monthly meeting. Why introduce the opportunity for bias to be introduced via revision of the investigation details without a trace? Nah. We can (and should) do better!
It is time a real discussion in this space is started.
Pete
November 2, 2024
Original Records
The new mullets.
Regarding FDA’s Guide for Data Integrity in CGMP, specifically Question 10: I feel that I need to do a bit of a deeper dive here, as there appears to be a disconnect between how industry and the regulator interpret this very important question. Sorry for the length, but I felt I had to cut/paste the entire section of the guidance into this blog for context. I have highlighted in bold the key words leading to confusion and ultimately unnecessary FDA Form 483 Observations. Here we go:
Q: Is it acceptable to retain paper printouts or static records instead of original electronic records from stand-alone computerized laboratory instruments, such as an FT-IR instrument?
PART 1:
A: A paper printout or static record may satisfy retention requirements if it is the original record or a true copy of the original record (see §§ 211.68(b), 211.188, 211.194, and 212.60). During data acquisition, for example, pH meters and balances may create a paper printout or static record as the original record. In this case, the paper printout or static record, or a true copy, must be retained (§ 211.180).
Thoughts:
“If it is the original record” – this is defined by PIC/s (FDA is a member) as the “first capture of information”. Meaning some computerized systems do not capture and store any data – it is simply transient:
older pH meters that simply display the value and create a printout, but do not store any electronic record of the analysis. The printout would be considered the original record. However, there are not many of these left: we might refer to them as CGMP Unicorns?
“or a true copy of the original record” – the process for creating true copies is defined in section 7.7.5 of the PIC/s guidance. The guide states that creating true paper copies of electronic records is “likely to be onerous in its administration to enable a GMP/GDP compliant record”:
This would require someone to periodically perform a 100% reconciliation between the paper printouts and electronic records. This individual would have to sign/date a worksheet or other record certifying that all data has been reconciled between the two sources (paper printouts and electronic). A second person would follow with another 100% reconciliation, and sign/date accordingly as a reviewer. Then the electronic database could be deleted by the IT administrator according to a written procedure, and the paper records could be considered true/exact copies. This is an “onerous” process, and really doesn’t make much business $en$e in any universe.
Additionally, there are many problems with this “true copy” approach, I will just name a few here:
The 100% reconciliation is taxing on front-line employees, and is a procedural control prone to mistakes. Serious deviations are likely, and will be an easy target for regulators.
There may be metadata that is not available on the printouts, but is associated with the original record. This means that true/exact copies are not being created, an easy observation…
You are demonstrating a quality culture that may have been acceptable in the “late 1900’s”, but certainly not today. It will be difficult for your site to survive much longer as quality transparency becomes standardized under FDA’s QMM…
PART 2
However, electronic records from certain types of laboratory instruments—whether stand-alone or networked—are dynamic, and a printout or a static record does not preserve the dynamic record format that is part of the complete original record. For example, the spectral file created by FT-IR (Fourier transform infrared spectroscopy) is dynamic and can be reprocessed. However, a static record or printout is fixed and would not satisfy CGMP requirements to retain original records or true copies (§ 211.180(d)). Also, if the full spectrum is not displayed in the printout, contaminants may be excluded.
Thoughts:
This section makes it seem that dynamic records are the only electronic records that need to be retained according to the record retention expectations. This is unfortunate. I totally get the “dynamic” example and how it helps put the situation in context, but in my opinion this section needs a revision; to clarify it is just an example. Although not in anyway incorrect, it appears to over-simplify what is a complex issue.
The key concept we must grasp to fully understand these first two sections is the concept of the “original record”. If you identify the “first capture of information” (typically electronic) – you then have a clear understanding of what must be done.
Many will argue that the original record on a pH meter or balance “lacks context” because results cannot be linked to specific samples. This statement may have some degree of truth, however, when it comes to the “C” in ALCOA, the history of testing can be very useful when evaluating historical testing for “orphaned data”. Unreported results have no place in a CGMP environment, and it is the role of the data owner to periodically (or frequently, depending on data criticality) monitor for the presence of such instances. This is a patient safety initiative. Context can be re-created if orphaned data is identified, with a nice FDA 483 as a bonus. Others might complain that without context, a CGMP procedure for adequate review cannot be completed. Again, there is of course some degree of truth in that statement, but certainly a simple reconciliation of results could be developed to prevent the presence of unreported results?
PART 3
You must ensure that original laboratory records, including paper and electronic records, are subject to second-person review (§ 211.194(a)(8)) to make certain that all test results and associated information are appropriately reported. Similarly, in microbiology, a contemporaneous written record is maintained of the colony counts of a petri dish, and the record is then subject to second-person review.
Thoughts:
Here we clearly see that the second person review again must be performed on the “original record”, which we now know is the electronic data and associated metadata. If you want to cling on to old habits, like the use of printouts, that’s OK – just don’t be under any illusions that these can be substituted for original records. Original records “are what they are”, either paper (limited instances) or electronic – you can’t choose!
In summary: be cool, follow the rule.
Original records are the new mullets (not the most eye appealing thing out there, but you just can’t not look)!
Pete
August 8, 2024
Thoughts on RCA
Today I was reviewing FDA WL 320-24-48 issued back on June 18th, to prepare for my investigation/CAPA workshop coming up in a few weeks. I was specifically focusing on point #2, failure to perform a thorough OOS investigation. I rarely deal with OOS investigations these days, as I mostly focus on DI-related deviations, and the stark contrast between these two types of investigations hit me almost immediately. They are totally different! The problem, however, is that top management may not fully understand the different approaches needed while investigating these two very different issues.
In both cases, identifying a scientifically-sound product impact statement and eventual CA-PA strategy is crucial. The acceptability of both of these regulatory expectations depend heavily on the ability to correctly identify the factor(s) behind the event, for example:
Without a strong understanding of the contributing factor(s), the scope may not be fully understood, leading to an inadequate product impact statement.
Without a strong understanding of the contributing factor(s), the proposed CA-PA may not prevent future occurrence.
Here, folks, is where the stark difference between these two categories of events resides:
1. For OOS investigations, a “root cause” can be identified and a explored via experimentation. Based on the results, a scientifically sound “root cause” can be determined and the investigation can continue… This is well defined in the regulatory guidance (phase 1, phase 2, etc…). If the sources of variability within a laboratory method are well understood, this process can be relatively straightforward.
2. For DI-related deviations, the situation is completely different. There is no “root cause” – that is certain. Trying to prove a “root cause” in a similar fashion as an OOS investigation will drive the QA department mad! They will be forced to operate outside the realm of science, more like science fiction. Interesting to read and highlights the authors’ creative ability, but not based in reality. Actually, there are a number of “contributing factors” that led to the event – a fishbone analysis may see factors identified in each branch. The level of effort put into identifying these contributing factors depends on the criticality of the event.
In summary, if management expects all investigations to be handled identically (for example following the OOS model of RCA), I’m afraid the Quality System may be stretched to is max, and may eventually break. So, what is the answer?:
A risk-based mindset led from the top, where the principles of critical thinking and flexibility are built in from the start. Timelines, compliance, and metrics come as afterthoughts when senior leaders focus on the process for investigations, rather than simply the outcomes.
May 26th, 2024
“Reliability”
How reliable is your data used for decision-making? FDA, in the opening section of their DI Q&A guidance, states that “FDA expects that all data be reliable and accurate”. In this blog post, I would like to explore the concept of reliability in two different ways, both in the context of GXP decision making:
Reliability in the sense that the data are able to be trusted/are dependable
Reliability in the sense that the data are statistically significant/representative enough to be dependable
In case #1, this generally applies to routine operations, for example, where defined procedures and practices are regularly evaluated by the regulators during inspection. The focus here is on building a risk-based data governance strategy (considering criticality) that demonstrates trust in the data (as much as is needed, considering the “intended purpose”), effectively managing the four sources of variability: hardware, software, personnel, and documentation. Expectations here are outlined in the PIC/s guide for data management as well as ICH Q9, and focus on the three pillars of governance: Design, Operation, Monitoring.
In case #2, this generally applies to the non-routine use of data within the “investigations” umbrella (OOS/deviation/complaint/etc.) of CGXP. How much data is enough to demonstrate reliability? Demonstrating reliability of data used in the investigation process (especially product impact evaluation) has been the Achilles heel for QA teams across the world for generations. This is without even mentioning the fact that that without a strong point #1 already established, point #2 was doomed from the start… Let’s assume for this blog that point #1 is well understood and properly managed.
Our best piece of guidance on point #2, in my opinion, can be found in section I.9 of ICH Q9, where the following statement is made:
“Statistical tools can support and facilitate quality risk management. They can enable effective data assessment, aid in determining the significance of the data set(s), and facilitate more reliable decision-making.”
When data is to be collated and used for non-routine decision-making, don’t forget that statistical tools can be a powerful tool for demonstrating the reliability of your decision, considering that the primary role of the regulator is to challenge the scientific justification for your conclusions! This is their obligation to the patient as a health authority… It’s not personal, just business.
With that said, focus on the business of demonstrating data reliability, both for routine and non-routine GXP operations – using statistical tools whenever feasible to justify why you do what you do. The business case for data reliability has long been proven across the spectrum of manufacturing. With data/metadata considered the “new currency”, don’t risk getting left behind (neither your organization nor your career)!
April 26th, 2024
“It is what it is”
The most important data is unknown and unknowable. This concept, attributable to W Edwards Deming, was made decades ago, yet still rings true despite the many technological advances we have made as a civilization. Just ask any front line employee tasked with managing day to day deviations!… No AI/ML model is going to come to the rescue here…. (although they may certainly help). It’s as universally fundamental as the first law of thermodynamics. “It is what it is” - forevermore, so to speak.
Essentially, the most important data would point us to a perfect process control strategy, which is, as we know from years of best efforts, impossible. It is sometimes managements supposition, however, that zero defects are indeed possible if employees would stick to the procedures and training. Wrong. Front line employees have little influence over Quality. Let that sink in for a moment…
Don’t let your management fool you on this point, or you will find yourself working in a miserable environment, struggling to meet questionable KPIs and wondering why you are failing. Losing sleep over something in which you have little influence. If the process could speak, it might say “it’s not you, it’s me”. As Deming once taught, employees have the right to be happy and find meaning in labor.
So what’s the answer? Ah! The regulatory roadmap has already been published = the two enablers found in ICH Q10, or what Dr. Deming once termed a “system of profound knowledge”. That’s the best we can do! If you find yourself in a company striving to build this system, you are in the right place. I bet you love your job! That’s a Quality Culture, enjoy it. Life is short.
Pete.
April 8th, 2024
“Level of Risk”
So… when is it expected that we identify the root cause related to an “unexplained discrepancy” (see 211.192)? Or when can we close the investigation with potential contributing factors (without identifying the “root cause” with some level of certainty)?
This question has caused us GMPers headaches for decades, due to the significant resources needed to dig down to the root. The Live Oak tree grows roots up to ~4 feet underground. Sometimes, depending on the investigation, a root cause dig can feel nearly impossible, much like digging 4 feet into our Texas rocky & clay-based soil! So, when is enough, enough – considering our limited resources?
Let’s take a look at a recent case study (drawn from an FDA Form 483 (Observation 1) issued 02FEB2024) for some insight:
The firm finds “unknown extraneous peaks” in cleaning verification swab results for what appear to be product contact surfaces (oral solid dosage).
Further analysis via LC-MS finds the identity of two peaks to be other drugs manufactured within the facility, with the remaining peaks being unidentified/unknown.
Investigations are closed without identifying the “root cause”, based on impact assessments and CAPAs.
The investigator concluded that the cleaning program was “deficient and unreliable” based on the findings summarized above. Namely, the failure to identify the “root cause”. Why were the impact assessments and CAPAs insufficient? Let’s look to ICH Q9(R1) for some guidance:
Firstly, the amount of effort we put into any investigation (211.192) depends on the “level of risk” (Q9).
The problem here is that we as an industry do not empower our employees to comply with this expectation. We often see the “zero defects” or “quality culture” on massive company posters accompanied with pictures of our patients, which translates to employees as we do not tolerate any risk to patient. Transparency with reality is not an option. There is no usable SOP to even refer to! As a result, we have to skip this step and hope that no regulator ever asks the question, with our fingers crossed that the level of effort we put into the investigation was OK. The truth is that there is increased risk, otherwise we wouldn’t have opened the investigation in the first place!
As an FYI here: risk is defined as the severity of a hazard occurring, combined with the probability or vulnerability of that hazard occurring. The tool used to determine this “level of risk” (Q9) varies (I recommend the qualitative nine-box methodology!).
In this case study, because the investigation was initiated due to carry-over residue of APIs and unknowns, it appears that the investigator considered the “level of risk” (Q9) to be high (severity of hazard * vulnerability). This is generally the case with cleaning (high * high) due to:
Severity: The unknowns that come with consuming impurities (think nitrosamines…) = high
Vulnerability: The highly manual and variable nature of cleaning (minus CIP) = high
The firm should have performed this calculation from the very beginning. We might refer to this as the North Star – guiding the investigation team through the process regarding the level of “effort, formality and documentation” (Q9). Management could have then dedicated resources to this particular issue, while diverting resources from other, lower risk investigations.
Without this initial calculation, or the ability to perform this calculation due to inadequate investigation SOPs, the investigation team is lost at sea. No North Star to guide them, and insufficient deckhands. The team will not know how far to dig (is 2 feet enough?), and management will not know how to “[free] up resources for managing higher risk issues” (Q9).
Lessons learned: Empower your investigation teams to follow the principles of ICH Q9(R1) – starting with determining the “level of risk” of any given issue. This small investment in employee development will reap dividends well into the future, by addressing the reality of risk, patient, and limited resources.
February 28th, 2024
Supplement the Swag
Boston is one of my favorite places on the East Coast. Something about the energy of the city inspires me. Maybe it’s the students packed into the bars and cafés solving the world’s challenges over bubble tea? Or maybe the Irish legacy of true hospitality through human connection? Maybe it’s a confluence of root causes. Either way, it’s cool, and a place to live in the moment.
At the Bruins vs. Kraken game last night, I struck up a conversation with the folks sitting to my left, a father and son, and once learning I was visiting from Texas, couldn’t help but make me feel right at home. Explaining the history of the team, and making sure my beverage holder was never empty. This place is simply inspiring and stimulates creativity in any visitor. As I boarded the plane back to Austin, I started searching the audiobook library for something to cap off my work week, and came across David Brooks’ latest work: “How to Know a Person: The Art of Seeing Others Deeply and Being Deeply Seen”. In the first chapter, David discusses his emotional awakening, and references several studies and publications along the way. One caught my attention, which I had briefly reviewed a year or two ago: the 2021 McKinsey study titled “‘Great Attrition’ or ‘Great Attraction’? The choice is yours”. I couldn’t help but make the connection to what the regulators are trying to inspire in both the Data Governance and Quality Management Maturity (QMM) initiatives. As I fly somewhere over western Virginia, here are my thoughts:
According to the study, “forty percent of the employees in our survey said they are at least somewhat likely to quit in the next three to six months.” Many of these responded that they would leave even without another job in hand… This suggests a significant trend in the post-pandemic working environment. Chatting with folks across the world in workshops and conferences (disclaimer: very limited sample size), I also notice a common thread that aligns with the McKinsey conclusions: a human search for purpose and meaning in labor. I feel an energy in the air when a team develops and presents a strategy for managing a hybrid system using a risk-based governance approach. Why? Because we have ditched the concepts of “inspection readiness” and “compliance”, and have rather unleashed critical thinking and focused on why we do what we do; we facilitated ownership.
You can feel ownership within five minutes of a facility walkthrough: folks are excited to present their strategy for managing their workflows. They are nowhere near perfect, but that was never an option anyway, and they understand that. They present a workflow that contributes to improving a patient’s quality of life, or perhaps even saving a life. Compliance and inspection readiness (old-school buzz words) create an environment of fear and uncertainty, because they command perfection. But we and our systems are all flawed, it is one of the universal realities. Remember the second law of thermodynamics from high school chemistry?: disorder only increases (or at least stays the same) with time!
FDA has spent over a decade researching the concept of Quality, and has had a few false starts (remember “Quality Metrics”?) along the way. In the latest attempt, we see the introduction of the five elements of Maturity. One of which is titled “employee engagement and empowerment”. I think we are now close to getting it right. Just read the mood in the room full of employees and you will understand why. I am sure many industry executives find this ridiculous [QMM], and have most certainly submitted comments against its implementation, as they cannot envision the connection between “empowerment” and “compliance”. This rejection [by management] aligns with the McKinsey study, as managers surveyed responded that the causes for employee departure were primarily transactional (e.g., search for better salary). Shocker: they were not.
FDA is first and foremost an agency acting to “protect and promote public health”. Drugs are manufactured and tested by employees, and our workflows are highly manual (and therefore variable). It is these employees that directly impact patient safety (not the C-Suite). Someone has to stand up for employees and (unfortunately) force management to take quality culture seriously, as it appears many sites remain siloed and disconnected. The “Quality Culture” mugs are cool (don’t get rid of them), just complement the swag with action.
Considering the current challenges to public health: drug shortages, severe departures from regulatory expectations, and continued globalization and supply chain complexity: the agency basically has two options to address the common root cause of poor manufacturing and quality practices (see recent FDA Warning Letters and 2019 Drug Shortage Whitepaper for any doubts). These two options are:
· Revise and enhance the GMP regulation (210/211)
· Revise and enhance regulatory guidance (the “C” in CGMP)
The latter is the obvious first choice, as it is exponentially more agile and allows for flexibility, considering the diversity of drug and biologic products. If this doesn’t work, however, the GMP regulation must be next. The ICH Q’s, DI/DG Guidance, QMM, and the Drug Shortage Whitepaper highlight the key enablers to achieve “employee engagement and empowerment”: here they are:
· Data Governance: workflow (vs. system) validation to achieve a “right environment” and meaning in labor
· Knowledge Management: building a library of knowledge to facilitate problem solving and stimulate innovation
· Risk Management: focusing limited employee resources on areas of greatest risk and reducing wasted efforts
An investment in people via the three enablers, in my opinion, addresses the faults found in the McKinsey study. Invest in compliance and you will see short-term benefits (e.g., GMP certification), but you will struggle to remain relevant in the future. Invest in people and you will reap benefits for generations and leave a legacy of good in this world.
February 8th, 2024
“One Wing and a Prayer”
plus: diamonds in the rough
Today I am having a little fun with the title of this blog entry… We have seen multiple recent FDA Warning Letters for OTC or other non-application products as the regulators around the world respond to catastrophic ongoing public health emergencies. These Warning Letters are for serious and basic failures, such as the lack of incoming raw material evaluation and/or lack of a process validation program (e.g., products containing glycerin).
Note: I did not use “lack of process validation”, as that would suggest that process validation is a one-time activity involving three batches and a report no one really ever uses.
You might initially dismiss these Warning Letters as not relevant learning opportunities for application-based GMP facilities, as I once did (to be completely honest). However, there is a wealth of knowledge regarding CurrentGMP expectations (diamonds) hidden in the rough (egregious basic GMP deficiencies). The most recent Warning Letter as of the writing of this entry is dated 31JAN2024 (WL# 320-24-18). Check out this guidance, and let’s break it down:
“You have not validated your manufacturing process used to produce homeopathic drug products, including those intended for infants and children. During the inspection, you indicated that you were not aware of the requirement.”
– Yikes! No comment here.
And now the learning part:
“…you must assure that your production process is capable of assuring all of your drugs are of acceptable quality, identity, strength, and purity. During process validation, the process design should be evaluated to determine if it is capable of reproducible commercial manufacturing.”
– Here we see FDA point directly to Design as the key ingredient to Quality assurance. The quality of commercial product is uncertain without a demonstration of good design principles. Passing the PPQ protocol requirements does not itself demonstrate good design. Rationale: PPQ batches are typically done under heavy scrutiny, as the are required for entry into the market, and are not representative of commercial manufacturing (e.g., volume/resources/etc.). A mature organization already knows this, so supplements these limitations with a plan for the future = “vigilant monitoring” (data & process mapping + qualitative risk assessment)
“A detailed summary of your validation program for ensuring a state of control throughout the product lifecycle, along with associated procedures. Describe your program for process performance qualification (PPQ), and ongoing monitoring of both intra-batch and inter-batch variation to ensure a continuing state of control.”
“This includes, but is not limited to, evaluating suitability of equipment for its intended use, ensuring quality of input materials, determining the capability and reliability of each manufacturing process step and its controls, and vigilant ongoing monitoring of process performance and product quality.”
– Here we see a focus on the “validation program” for PPQ batches and commercial manufacturing, as discussed earlier.
Q: How can we demonstrate adequacy of the “validation program”?
A: Via knowledge of the variability inherent to each process step (remember the DI guidance? variability arises from the four scoundrels: Hardware, Software, Personnel, Documentation).
What you plan to vigilantly monitor depends on the outcome of your variability assessment (aka risk assessment)! Again, this is necessary because of the non-representative nature of PPQ batches.
– Let’s be honest, there is no way to determine the capability and reliability of each manufacturing process step and its controls via a traditional PPQ protocol/report. If we rely on this report alone, we might refer to that as a “wing and a prayer”.
FYI (a bit of history here): “a wing and a prayer” probably originated from the film Flying Tigers (1942), where planes were barely able to return to base after flying over the “hump” or Himalaya range as they brought in supplies to China during WW2, hence: “coming in on one wing and a prayer”. We cannot enter commercial manufacturing on “one wing and a prayer” - we can do better than that!
Conclusion: Process Validation is how we demonstrate quality, despite all the unknowns that come with batch manufacturing (meaning we cannot test each individual unit). It is a combination of development and design experimentation, risk management, traditional GMP controls, psychology and culture. What it is definitely not: a compliance report that simply consumes energy on some server in an attempt to be “inspection ready”… Honestly, I think we need to start moving away from that term “inspection ready” – it causes unnecessary fear and panic among staff, which never adds value. Just be confident in your processes and inspections will become an afterthought.
January 21st, 2024
Compliance?
As I was reading a recently published FDA Warning Letter dated 21NOV23 (for what must have been the tenth time – this one is full of insight…), specifically section 2B, outlining the firm’s failure to investigate NVP excursions, I was immediately consumed with concept of “compliance”. This particular Warning Letter is an extensive insight into the rationale behind the C in GMP – what it means and where it is going, specifically on the topic of data governance and the rationale behind this expectation.
According to the letter, the firm had established a permitted NVP excursion buffer, meaning that an investigation would only be performed if the alarm persisted for some defined timeframe. I am sure they had established procedures to ensure DI and ALCOA+ were evaluated, and had a signed and archived “DI risk assessment” somewhere in the quality system. Most if not all sites already have this program and (unfortunate) checklist in place. I imagine internal audits and inspection readiness checklists were completed with 5 stars, but no one bothered to evaluate governance of the process and ultimate decision-making (in this case to release a DP). An ALCOA+ evaluation will pass this scenario every time, but a governance approach would have failed. This gives the site a false sense of inspection readiness. Governance is ALCOA+, plus an evaluation of good decision-making. Regulators are now expecting both – which we could define as CGMP.
Let me expand on this:
Governance would have required applying the ICH Q9 vertical flowchart to each step/interface in the NVP process. One of the hazards (HI) identified would have been potential product contamination in the case of an NVP alarm. No way the firm could have actively accepted that risk, as the severity would be “H” and the probability would be unknown, defaulting to either “H” or “M” (depends on many factors). Either way, using the “nine-box”, we would have a high risk hazard, triggering a procedure that requires an investigation (especially as we are in the final step of DP manufacturing…). However, and unfortunately, it is unlikely the governance approach was applied, allowing the firm to settle on an ALCOA+ compliance checklist – with a 50% inspection score (fail). This was passive acceptance of risk – which was deleted (rightfully so) from Q9 and is no longer an option in R1. This is worrying: that basic risk management (2005) and governance principles (2021) are still gathering dust on the internet, despite being around for almost (at least in the case of Q9) a generation!
The reason for issuing QRM, data integrity and data governance guidance provided by the regulators over the past 19 years is not simply some random compliance expectation. If a firm does not understand the rationale behind compliance, they are unlikely to survive much longer, especially as QMM comes into force. Compliance is not the ultimate goal of CGMP: never has been and never will be: it is a way of doing things, thought processes, critical thinking tools, and culture. The ultimate goal is good scientific decision making, and decisions are made by humans evaluating data via some process that has inherent risks… compliance is simply a prerequisite. Compliance is (perhaps?) GMP, but compliance is not CGMP.
Always remember – quality always ensures compliance, but the reverse is almost never the case.
Let’s go!
January 8th, 2024
A Quality Framework:
AI/ML
This blog entry was written by myself, along with Ulrich Köllish and Jennifer Roebber, GxP-CC GmbH, and originally published on bioprocessonline.com.
As the use of AI/ML in society has increased exponentially in the past few years, primarily because of increased availability and reduced costs of implementation, it is natural to expect its eventual and rather slow introduction into the GXP world. GXP users are generally slower to introduce new and disruptive technologies because of the heavily regulated nature of our business processes and low tolerance for risk/uncertainties. AI/ML has been used in drug discovery for some years and to some extent the GLP/GCP environments; however, it has not yet been adopted by the GMP commercial community.
Recently, the FDA published a discussion paper on AI/ML in drug manufacturing and solicited feedback from industry. The industry’s comments show that an important factor preventing AI/ML implementation lies in a lack of regulatory guidance for the unique aspects of AI/ML not covered by existing computer system validation, such as, for example, minimizing bias in models, data protection, and quality for model training. Limited industry guidance, at least, has been proposed and outlined in the ISPE GAMP 5, second edition, published in July 2022.
In 2023, FDA published two discussion papers in an attempt to gather industry’s views on additional use cases, implementation blockers, necessary data management activities for implementation, and other comments that may be useful as the agency develops more concrete guidance. Also, in 2021, the FDA's medical device division (CDRH) published AI/ML guidance, which we believe is much aligned with the existing pharmaceutical data integrity and risk management framework of subjectivity, formality, and decision-making. For example, the 10 guiding principles forming the Good Machine Learning Practice for Medical Device Development parallel the existing CDER guidance for three-stage process validation, published back in 2011. We expect that the guidance for pharmaceutical products will follow a similar path, with future guidelines echoing risk management within the existing cGMP framework.
In this article we discuss guidance already available that provides an excellent foundation for the eventual GMP AI/ML revolution, with the goal of preparing industry for future implementation while minimizing future growing pains. Waiting for further guidance to establish an AI/ML framework from the regulators to get started would represent a serious mistake, as the journey is a marathon rather than a sprint. As such, we propose taking action now via the following three steps:
Before we can begin to develop a pathway forward, we must remember the difference between qualification and validation. In the case of AI/ML, we would speak of qualification in the context of the model or platform itself, and validation as the use case in the context of the overall business process, including the process, the environment, and the operators. FDA, in its guide for data integrity, cites validation for intended use including “software, hardware, personnel and documentation.” Qualification provides the scientific evidence that the model functions appropriately within the Good Machine Learning Practice framework (yet to be defined by CDER, but likely following on the heels of the CDRH SaMD guidance), while validation demonstrates that risks arising from the use of the model in a GXP environment are controlled according to its “intended performance.” Demonstrating either of these requirements during regulatory inspection is tricky for AI/ML and likely must rely heavily on risk management. The burden will be on the company to demonstrate how the use of the model within the validated process does not add unnecessary risk to patient safety (meaning better than the status quo). Considering this burden, a black-box defense will likely not be tolerated, as it does not mitigate the potential for risks such as biases in model performance.
Step 1: QRM And Intended Use
A solid quality risk management (QRM) framework within your network is essential, as the intended performance requirements of AI/ML will vary greatly depending on patient proximity, from upstream process control (generally lower risk) to downstream QA decision-making (higher risk). Experience using new tools, such as the informal/semi-formal and qualitative tools (e.g., data and process mapping) pushed in the new ICH Q9 revisions during routine legacy GMP operations, will pay dividends in the future, as it allows the SME to clearly explain the intended performance of the model during regulatory inspection, greatly reducing the potential for confusion and misunderstanding. In the same sense, quantitative and formal tools relying on multiplication of risk categorization impede critical thinking and will likely ultimately fail to produce the rationale necessary to fulfil the burden of intended use.
Step 2: Data Governance And Acknowledging Bias
In any industry adopting AI/ML applications, a solid data governance program is a prerequisite. No amount of good machine learning practices can address unknown biases in the data sets to be used for qualification and any future decision-making. Luckily, the road map to success for governance has been clearly outlined in the PIC/s guide for data management and integrity (design, operation, monitoring). Good data governance does not mean that bias is eliminated but rather acknowledged, reduced to an acceptable level (if necessary), and regularly monitored.
According to the State of MLOps Industry Report 2023, “over a quarter (27%) of ML practitioners surveyed believe that bias will never truly be removed from AI-enabled products.” So, it appears the goal is not to demonstrate freedom from bias (perfection) but rather to identify sources of bias and acknowledge limitations in the model output accordingly, which happens to be the same goal described under the PIC/s data governance guidelines.
In anticipation of AI/ML in future applications, we also recommend dedicating significant resources now to strengthen governance programs that go above and beyond minimum GMP requirements. Creating new roles within your organization such as a chief data officer to propose strategies for use of your data, assigning ownership and responsibility to data sets, and management’s promotion of an overall data culture will provide the governance foundation necessary to benefit from any future AI/ML use cases.
Step 3: Development Of Internal AI/ML Standards And Quality Oversight
In our recent experience, we have found that many companies are already well into qualification activities for AI/ML models, which is in-line with published use cases from natural language processing to QC data trending to digital twin However, our conversations demonstrated that most sites are currently just beginning the process of establishing AI/ML frameworks within their quality system and developing as they go. By not preemptively establishing standards, these companies are making the future defense of the model for its intended use difficult as there is limited ability to recreate the qualification activities using scientific evidence (e.g., documentation). We foresee a difficult journey ahead if the quality unit is not involved from an early stage, implementing a standard set of expectations that must be followed.
We recommend implementing a good AI/ML standard prior to initiating development activities, so that any knowledge about the model gathered during early development can be referenced within the risk management program alongside some Quality oversight. As is well understood within the AI/ML community, one of the biggest risks is model bias, which comes in different forms and can arise at different points within the model development. We anticipate that the inability to produce documentation regarding the prevention of bias during model development will be a significant source of regulatory concern. As AI/ML is designed to drive future decisions regarding events that are likely to occur based on what the model “learned” from its training data, we have to demonstrate that the way the training data was collected and selected was unbiased – meaning free from influence that would cause the model to no longer meet fundamental scientific standards. An analogy can be drawn to human behavior: it is well understood that employee training in any particular activity is heavily influenced by any bias the trainer exhibits during the training activity, such as, for example, a dislike for a specific action outlined in the SOP. Demonstrating that the model is free of bias can be tricky and very high-risk – as evidenced by the many established case studies in society where bias in AI/ML has caused serious harm. On the bright side, once we develop QRM maturity, implement good risk-based governance, and roll out a standard framework with Quality oversight, AI/ML becomes feasible and, in our opinion, will greatly enhance the quality of medicines via multiple means yet to be discovered.
Conclusion
The potential applications of AI/ML in drug manufacturing are meaningful and will lead to reduced errors, recalls, and drug shortages. We see AI/ML as a needed tool to overcome current life-threatening situations and so much more than just a cool new technology. FDA’s Drug Shortage report from 2022 describes a dire situation with regard to access to essential medicines, with shortages increasing 30% as compared to 2021, with 62% of these shortages due to quality and manufacturing issues. Surely, new cGMP solutions are necessary and cannot wait – patients are waiting, literally. Our recent conversations with some in industry have been promising, and we are excited to see this transformation already underway. With a few minor additions to our existing quality system referencing existing regulatory guidance, we can be sure the future is bright.
December 18th, 2023
Validation
From a CPV perspective
Regarding “Validation” in the context of GMP:
Let us start with the definition. After querying Merriam-Webster, I was able to find two meaningful extracts relevant to this blog:
1. To support or corroborate on a sound or authoritative basis, and
2. To confirm the validity of.
If we look to the regulations (Parts 11/211), we find a total of eight instances where a variation of the word “validate” is cited. For this blog, we will focus on those two instances specifically referring to what we have now come to term Computer System Validation “CSV” – Part 11.10(a) and Part 211.68(b). These regulations refer to expectations for commercial manufacturing, and we will use the concepts of FDA’s Process Validation Guidance (specifically stage 3 “Continued Process Verification” (CPV)) for this discussion. CSV, in actuality, is a term used to describe the individual activities of software/hardware “Qualification” (e.g., IQ/OQ/PQ), in an attempt to facilitate a systematic means for compliance with these regulations. It is assumed that once these individual software qualification actions have been performed successfully according to a pre-defined protocol, the system is “validated” and can be used in commercial manufacturing. Decades of past regulatory action and public health tragedies including drug shortages, however, lead us to believe this is a false assumption.
Let’s go back to basics for a moment and simplify what has become (in my opinion) a large contributor to the ~62% of drug shortages attributable to “manufacturing and quality issues” = failure to embrace the true principles of stage 3 process validation (CPV) and instead focus on individual compliance tasks within disparate department siloes all the while making unfair assumptions in high risk manufacturing areas. We have failed in our attempt “to support or corroborate on a sound or authoritative basis” that our products are safe and effective! Why? Because we have only completed 50% of the job. During inspection, the regulator will be looking for two things during an evaluation of any given process:
· System Qualification (Hardware and Software)
· Workflow Validation (Hardware, Software, Personnel and Documentation)
Note that the Workflow Validation simply references the System Qualification when necessary, while addressing in detail the Personnel and Documentation components. For a detailed explanation of Workflow Validation expectations, check out Q3 of FDA’s Data Integrity Guidance. Once we break it down into these two concepts, and finally align with regulatory guidance (e.g., CPV), we can now properly define the efforts needed at the design, operation, and monitoring stages within routine commercial manufacturing that need to be addressed with regard to both bullet points. Old school CSV has a healthy serving of System Qualification, but zero Workflow Validation. The inspection grade is 50% (an F).
Folks in the CSA camp have tried to define the reduced efforts needed at the System Qualification stage via a risk-based approach, but I fear they are missing the scientific justification: a link to the Workflow Validation. Without this link, the intended use is unknown, and therefore a risk-based approach cannot be justified. This will be seen as an opinion by the regulator (without the link), which may be the reason CDER did not sign off on the guidance: perhaps is tries to simplify and standardize a concept that requires critical thinking and a case-by-case evaluation…?
The two concepts are attached at the hip and fully reliant on each other to provide your scientific rationale during inspection. Don’t be fooled here, CSA cannot be used as a means to standardize your qualification efforts via a decision-tree! As humans we LOVE checklists, flowcharts, and really anything that make our lives easier (TNTC examples here). I’m afraid, however, that there are no shortcuts available here: don’t fall into the trap. We will have to use critical thinking and proceed on a “case by case basis” – to steal the working from Q9.
I am feeling bold this evening as I fly somewhere over West Virginia: I would propose we scrap the concept of CSV altogether. Leave it in the back storage room alongside the dot matrix printers we used to print and weigh chromatography peaks. Looking forward to 2024, they should both exist in glass cases within your local technology museum. I am not questioning the value of Qualification, but rather the assumptions that come with “CSV”. Regarding these assumptions, and to provide further evidence, I see a direct conflict with two existing FDA Guidance Documents:
1) Process Validation (2011): “The goal of the third validation stage is continual assurance that the process remains in a state of control (the validated state) during commercial manufacture.” CSV is generally a one and done activity.
2) Data Integrity (2018): “Controls that are appropriately designed to validate a system for its intended use address software, hardware, personnel, and documentation.” CSV only addresses hardware/software.
3) 21 CFR Part 11.10(a): “Validation of systems to ensure accuracy, reliability, consistent intended performance, and the ability to discern invalid or altered records.” CSV does not consider the intended performance (aka workflow).
I struggle to find any significant modern regulatory publication/guidance related to pharmaceutical manufacturing that aligns with CSV. As an investigator, I was provided with countless examples of industry publications on the matter, however, as a regulator I was not interested in an opinion of what CSV should or should not entail (with the exception of the lunch breaks); there is no time for such discussion during a time sensitive inspection. I simply used the guidance listed above to determine if the processes that were directly influencing patient safety were under a sufficient level of control according to risk management principles outlined in ICH Q9. This is demonstrated via an evaluation of the following components of any given process: hardware, software (Qualification), personnel and documentation (SOPs/training/batch records/forms/etc.).
I understand that this is a paradigm shift, and as humans even small shifts are terrifying – but we must tackle this misunderstanding (with best efforts to be as non-invasive as possible) and re-calibrate the way we as an industry understand and implement “validation”. The concepts of true validation as outlined by the regulators are not hard to understand, but anytime change is necessary we must see value to create motivation. Success is determined by a combination of resources and motivation. Resources are provided by executive management, and motivation must be self-generated by staff tasked with executing the work. In theory, motivation should be easy for us considering the life-saving products we manufacture, but we have allowed compliance to spoil it. Some may place this blame on the regulators, but the concepts of risk management have been around for over a decade. Every site I visit around the world is filled to the brim with potential and motivation. Don’t let an outdated interpretation of compliance get in the way of world class manufacturing.
Never implement significant organizational change without careful planning, which almost always should include execution of a pilot study. The pilot is performed not only to evaluate the immediate result of the change, but equally important evaluate its effect on employee motivation and reduce the anxieties that come with significant change. It’s a simple litmus test: did the change create an environment that will motivate staff to find purpose and meaning in labor? If yes, let’s go! If not, it’s back to the whiteboard.
Now back to validation… When Workflow Validation and System Qualification come together to form our control strategy for CPV, we can achieve the following, which I have no doubt will improve motivation:
System Qualification: The least burdensome (aka risk-based) qualification approach is taken (including screen shots/etc.) based on those areas within the workflow that are of highest risk to our patients. When a script is executed or a screen shot grabbed, it is because it matters, a confirmation is needed because our patients depend on a right first time strategy. This lack of dilution brings purpose and meaning to the activity = motivation.
Workflow Validation: Procedures, logbooks, training, worksheets, batch records, and other control strategies are established using the least burdensome (aka risk-based) approach. When an audit trail review is required, it is because it matters, a review is needed because our patients depend on a right first time strategy. This lack of dilution brings purpose and meaning to the activity = motivation.
Further Reading: Paste into Google (or your preferred search engine): “FDA Warning Letter Inter and Intra Batch Variability”
Once critical thinking and motivation is allowed to flourish, and executive management are on board, now we can talk “Quality”
- Pete
November 15th, 2023
Knowledge Management
“it’s a no-brainer”
OK, so what exactly is knowledge management (KM)? It seems like we should cover it here since Q10 has become the hottest topic in our industry at the moment as FDA moves forward with the QMM protocol assessment in response to increasing drug shortages. Q10 is finally getting the attention it deserves, what a pity that it took over a decade…
Just for background, KM is one of the two “enablers” within ICH Q10 that may permit a site to achieve an advanced (or mature) Quality System. This is a site who reliably produces high quality medicines “without extensive regulatory oversight”.
The concept of KM is defined in ICH Q10 as follows:
Product and process knowledge should be managed from development through the commercial life of the product up to and including product discontinuation. For example, development activities using scientific approaches provide knowledge for product and process understanding. Knowledge management is a systematic approach to acquiring, analyzing, storing, and disseminating information related to products, manufacturing processes, and components. Sources of knowledge include, but are not limited to, prior knowledge (public domain or internally documented); pharmaceutical development studies; technology transfer activities; process validation studies over the product lifecycle; manufacturing experience; innovation; continual improvement; and change management activities.
Sounds great, but a definition without practical examples is difficult to envision, especially when operating within a highly regulated environment and very limited resources. I have been focusing on this concept for the past few months, trying to develop a means for explaining KM that is “non-invasive”, so as to not disrupt ongoing operations. I have come to the conclusion that KM can be implemented in various ways, however, in my opinion, the most efficient and effective way is to capture knowledge (explicit and implicit) within our workflow validation packages (see Q2 of FDA’s Data Integrity Guidance). A workflow validation package includes consideration of hardware/software/personnel/documentation, and implements a risk based strategy for ensuring the accuracy and completeness of data via the three pillars of governance: Design – Operation – Monitoring
Example #1: An analyst knowing that an extra minute of sonication during sample preparation reduces variation in assay results is potential knowledge that can be integrated into the quality system to reduce OOS’s and drug shortages. However, this will remain “information” in the analyst’s head until there is a management strategy in place to document this implicit information within the workflow validation risk assessment, at which point it then becomes knowledge. Information does not become knowledge until it is documented, and the most efficient capture of this information is within a workflow validation risk assessment! This forms the library of knowledge that can be used throughout the organization when needed (in this case, during an OOS root cause evaluation). The ability to assign a potential root cause by referencing the KM library will improve efficiency and demonstrate the “scientific rationale” necessary to perform re-testing/sampling.
Example #2: It is explicit information that failure to rinse the probe prior to pH analysis will cause contamination of the sample, lowering the pH and possibly resulting in an OOS. This is just science. This will remain information, however, until there is a management strategy in place to document this implicit information on the workflow validation risk assessment, at which point it then becomes knowledge. This forms the library of knowledge that can be used throughout the organization when needed (in this case, during an OOS root cause evaluation). The ability to assign a potential root cause by referencing the KM library will improve efficiency and demonstrate the “scientific rationale” necessary to perform re-testing/sampling.
Without a KM library to reference, the regulators often conclude the firm is relying on their opinion to justify root cause conclusions/product impact statements/rationale for re-testing/other critical GMP functions. This is the “root cause” of TNTC 483s!
It is time to get on board with KM – it’s a “no-brainer” 🥸
October 15th, 2023
QMM Updates
Objectivity
FDA has recently published an update on their ongoing development of the Quality Management Maturity (QMM) assessment protocol, which has further refined the elements to be included in the evaluation of a site’s advanced pharmaceutical quality system (PQS). The Agency has outlined five elements that are likely to be included in the eventual assessment protocol:
1. Management Commitment to Quality
2. Business Continuity
3. Advanced Pharmaceutical Quality System (PQS)
4. Technical Excellence
5. Employee Engagement and Empowerment
These elements should come as no surprise, as they have been communicated in some form in previous QMM and/or drug shortage publications; and are fully aligned with the principles already described in ICH Q8, Q9 and Q10. The question is not the value in investing in such elements, but rather how to perform an objective evaluation and ensure consistency, considering the diversity of manufacturing processes and varying levels of resources available to manufacture different product classes (e.g., generic vs. innovator).
This will no doubt be the biggest challenge to implementation of the program, and will eventually have to settle on achievable goals for each element. In my opinion, this will include an evaluation of the tools provided to site staff to achieve success in each area (it will not revolve around how well site management can speak to the elements) – but rather what are you doing about it. One meaningful management metric for element #4 might be “number of human hazards existing within our CPP/CQA workflows”. Success in each area will depend on the effective use of the “enablers” outlined in Q10:
1. Knowledge Management (effective utilization of unstructured data/information)
2. Quality Risk Management (focus on design, operation, and monitoring of key workflows)
For those sites operating with limited resources, you might be wondering if you can compete within the eventual QMM program. The answer is = absolutely.
Answer = By embracing and investing in the principles of “Non-Invasive Data Governance”, each of the five elements above is addressed through efficient use of limited resources. It involves two key principles:
1. Integrating existing processes into the formal Quality System
2. Re-directing existing resources to achieve process ownership (away from non-value-added activities and into Quality-focused-activities)
Disclaimer: As a training company focused on element #5, I obviously have a conflict of interest here.
I’m excited to see how the QMM protocol evolves, especially as they try to tackle the problem of objectivity. If they design the protocol to include a measurement of how the site actively works to reduce risk to patient safety (drug shortages + safety/efficacy) through the introduction of new QRM and KM tools, then I believe this years-long initiative will result in a significant return on investment.
September 30th, 2023
15 Years!
Dr. Califf Visits India
This past week FDA commissioner Dr. Califf was visiting India to celebrate 15 years since the establishment of the New Delhi office, a place that holds special meaning for me. As a result, I was interested in the details of the visit, and one particular activity caught my attention: Dr. Califf’s 25 minute sit-down interview with CNBC’s “The Medicine Box” on September 29th. I was impressed with the direct and meaningful nature of the questions. It was evident that the journalist was well aware of the current compliance environment, and unafraid to ask tough questions! The interview covered several hot topics:
Unannounced Foreign Site Inspections: my take on the interview is that we can expect these to continue and most likely be expanded, especially because Dr. Califf actually states “I think a mixture of announced and unannounced is important, and you will see more unannounced inspections.” Essentially, no firm should now be surprised if an FDA Investigator shows up in a foreign facility without notice, especially anywhere the FDA has a permanent presence (EU, South/Central America, Asia), which makes the logistics of such a visit easier to manage.
Re-Shoring Essential Manufacturing Capabilities: FDA has little influence on the factors that could encourage re-shoring, as a science-based public health agency. Economics has a large role to play here, among other things outside of the FDA’s control.
Emerging Concern with Clinical Data Integrity: Dr. Califf himself inserts the “including clinical” comment several times as a concern, including when responding to questions about post-COVID compliance. This is notable considering the recent press regarding the reliability (or not) of clinical trial data being used to approve drug applications. This is a worldwide concern and potential nasty can of worms about to be opened. Be prepared for a crackdown on enforcement of good clinical data governance. See my earlier blog post for an evaluation of the recent European guidance for GCP data management, which provides excellent advice and is largely harmonized with previously published commercial DI guidance.
Maturity: Dr. Califf emphasizes a focus on the transition to digital, which could aid the agency in determining when and where to perform inspections, as well as specific areas of interest in which to focus during those inspections. We are likely some years away from such a scenario, but the comments fit in quite nicely with the recent FDA update earlier this month to the QMM journey and potential rewards for Quality investments, which they have been pushing hard the past few years. In parallel to the discussion on digital transformation, there is an emphasis on employee training and empowerment, a necessary ingredient for true Maturity. Industry should be prepared for a change in tactics when it comes to the FDA evaluation of employee training programs, with an emphasis on the ability to demonstrate training effectiveness, rather than simply providing evidence that training was provided.
I could keep going here on the link between the interview and industry’s QMM journey – but will save that for the next Blog post, stay tuned!
September 12th, 2023
Objective 4
Updates to FDA’s Pre-Approval Inspection Program
FDA’s “Compliance Program Guidance Manual” (CPGM) 7346.832, which provides an in-depth guide for the investigator on factors to consider when performing a “Pre-Approval Inspection” (PAI), was revised in October 2022 with little fanfare. This is surprising, considering the significance of this CPGM to the overall application approval process. The previous guidance had been released in August 2019, and was effective for just over three years (a very short lifespan for regulatory guidance!). Interestingly, the PAI program was an outcome of serious fraud and corruption uncovered in the mid 1980’s, commonly referred to as the “generic drug scandal”. The program was designed to prevent fraudulent applications from gaining approval via a vigorous on-site inspection. The inspection outcome performed according to the CPGM, combined with the expert review of the various application components, come together near the end of the process to inform the overall approval decision. The PAI process has long included the following three traditional objectives:
Objective 1 - Readiness for commercial manufacturing: is the firm capable of producing the drug at commercial scale, or will the site struggle to maintain a consistent supply, resulting in drug shortages?
Objective 2 – Conformance to Application: was the process, equipment, and other factors consistent with what is observed during the on-site inspection?
Objective 3 – Data Integrity: were the data submitted in the application accurate and complete?
Firms have traditionally prepared for evaluation of these three objectives the best they can, considering the investigator will likely take a risk-based approach to coverage of each objective.
What stands out in this new revision is the addition of a new objective, titled “Objective 4 - Commitment to Quality in Pharmaceutical Development”. This objective is a break from the traditional compliance approach to inspection, and is aligned with other recent FDA whitepapers, namely FDA’s vision for Quality Management Maturity (QMM). This objective appears to be an attempt to gauge the level of maturity within the firm’s product development program, with two keywords standing out: knowledge management and quality risk management. For the regulator (and patient), these ingredients are important, considering the approval process is largely based on trust: the expert review and inspection activities only evaluate the tip of the much larger product development iceberg. Has the firm been transparent with all relevant development outcomes? Again – the process is largely built on trust, which can be tricky considering human nature – namely the universal faults with regard to conflict of interest and cognitive dissonance!
How can we limit these universal human flaws? The answer comes in the form of systematic tools for capturing knowledge (knowledge management) and evaluating that knowledge through the patient safety lens (quality risk management). Without firmly established and mature tools, bias is allowed to creep in like the cockroaches of central Texas… and the result is unpleasant for everyone involved.
Speaking of systematic tools, ICH Q8 “Quality by Design”, which has been around since 2006, provides a harmonized guide for building quality into the development process, so in reality the addition of objective 4 and the evaluation of a firm’s maturity should come as no surprise… Any grace period needed to adapt the concepts behind Q8 into a given development program has long since passed.
A quick self-evaluation can be performed to gauge one’s inspection readiness for 2024:
Knowledge Management: Has management provided the solutions necessary to ensure information gathered during development can be transformed to knowledge via digitization? To gauge one’s maturity, use the FAIR principles as the standard for success.
Quality Risk Management: Has management updated the overall QRM program in line with last year’s revisions to ICH Q9? To gauge one’s maturity, use the spectrum of formality with regard to available QRM tools (from a risk memo to FMEA) as the standard for success.
This is already a long post for a blog, and my flight is landing soon, so I will wrap it up here: In summary, management investment in the product development program should be sufficient to allow adaption to updated regulatory guidance. If data are still captured on paper (or paper on glass), your firm runs the risk that a poor maturity evaluation may lead to a loss in confidence regarding the accuracy and completeness of your application. This will likely lead to delays in product approval until additional verification can be completed either through written correspondence or a follow-up secondary on-site/remote inspection. Consider the approval process from the regulatory/patient perspective and the iceberg analogy, and it really is a “no-brainer” – a mature quality system within development (don’t worry, this is different than commercial GMP) is no longer optional. It’s time to implement flexible and risk-based tools that will unleash critical thinking throughout your organization and bring high-quality medicines to patients without regulatory delays.
June 18th, 2023
Formality
As I was reading through a recently published FDA Form 483 issued on 12 Aug 2022, the following statement caught my attention: “a patient death occurred while using the…” Reading through observation one, we find that the device had reached its “upper limit of notifications that can be transferred”, causing a delay of ~one week (transmissions were supposed to occur daily).
I immediately began imagining what tools the firm used for Quality Risk Management. Just like in the garage, the ability to fix anything well depends on the tools provided to the mechanic (it’s generally not the mechanic, but the resources available within the garage that matter most)! If the mechanic is only provided a multimeter to fix an electrical fault, then the outcome of the repair will be in commensurate with this limitation. The mechanic will struggle to remove the parts necessary to access the full electrical system to determine potential faults. In my experience, sites that have world-class risk management programs are those that take advantage of the full spectrum of formality (see ICH Q9(R1)), just like a mechanic should have full access to a wide variety of tools, from pliers (less formal) to a multimeter (more formal).
I wonder if combining less formal tools (data & process mapping) at the hazard identification stage with more formal tools at the risk mitigation/acceptance stage could have led the site to identifying, mitigating and controlling this critical risk appropriately? PIC/s provides an excellent roadmap within their guidance “ASSESSMENT OF QUALITY RISK MANAGEMENT IMPLEMENTATION”, which states:
“The QRM process normally consists of several steps including:
Process mapping identifying all inputs, outputs and existing control measures;
Risk Assessment (incl. risk- identification, risk-analysis and evaluation);
Risk Control (including risk reduction and risk Acceptance);
Communication (i.e. the residual risk should be communicated to the regulators and customers);
Regular Review of the risks”
When a site is provided only the most formal tools (multimeter) – they are generally not able to trigger the critical thinking necessary for a successful QRM strategy. Just like the mechanic will never be able to remove the machine parts without the pliers (now only the ability to access the main battery)… What’s in your site’s toolbox? Do you have the full spectrum of tools necessary for success? Don’t be afraid of less formal tools – take another look at ICH Q9(R1) section 5.1 to gain the confidence necessary to expand the tools in your garage – it will pay dividends well into the future.
Perfection was never an option - just do the best you can with the resources you have and you will suddenly find yourself operating a world class manufacturing operation.
May 4th, 2023
Artificial Assistance
As I was addressing audience comments submitted following my recent webinar on Quality Intelligence, the question was posed: “can you comment on the importance of Artificial Intelligence and Data Analytics in drug manufacturing?” During my response, I stated that “advanced data analytics will allow our industry to improve process control strategies in ways we cannot comprehend without artificial assistance”. Artificial Assistance? Surely someone has termed that phrase, so I Googled it, but alas – Google did not provide me with a definition, but rather directed me to links advertising various artificial assistants (totally different thing, but very cool!). I was hoping to reference another trendy term in this new world where AI and the pharmaceutical industry convergence, but no such luck.
The reason I felt compelled to Google the phrase was that as the two words appeared on my screen, I immediately felt that it described the “intended use” (see 21 CFR Part 11.10(a)) of the various AI tools within our heavily regulated industry. When we define the intended use, we can then proceed with a validation strategy. We can feel confident moving forward alongside AI solutions, addressing the validation hurdle by considering how these tools are to be used: artificial assistance. One example that comes to mind: AI will enhance (or “assist”) the human (QA) to ensure that the final batch disposition decision is based on our best efforts of analyzing the data set for any indication of a quality defect. In this context, the validation burden becomes manageable using existing qualitative risk-management tools outlined in ICH Q9, considering the “intended use”. Risk to patient safety introduced from use of these tools can be managed by demonstrating that the decision (disposition) will not be based solely on the outcome of an AI algorithm alone, without human verification, but rather an enhancement of traditional human data review and approval processes alongside an artificial assistant that improves the disposition process in a demonstrable manner.
Two is always better than one!
It would be foolish to move ahead with the attitude that AI will not introduce risk to the example mentioned above, but why would we let risk prevent us from improving the process? No great innovations come about without confronting new challenges. By acknowledging and managing risk, humans have been improving processes since the beginning of time! All innovations present new and different hazards, but lucky for us a clear and concise roadmap for risk management has already been provided by the regulators!
We already have the tools - so let’s get started!
March 31st , 2023
Uncertainty & Assumptions
Failure to perform adequate investigations into "unknown discrepancies" continues to be the #1 cited GMP regulatory observation, year after year, often leading to unfortunate regulatory action (e.g., Warning Letters & recalls). The regulation requires discrepancies to be “thoroughly investigated”, but how thorough is thorough enough? To answer this question, we must reflect through the lens of the modern CGMP. To do this, we need a clean break with the past. Past pitfalls that have led to regulatory problems can generally be attributed to the failure to address and rationalize uncertainty and assumptions that were included in the investigation (scope, root cause, product impact), causing the end result (conclusion & CAPA) to fall short of regulatory and patient expectations.
The modern CGMP Quality System, especially considering the tools outlined in ICH Q9 (R1), does not allow one to:
1. Leave uncertainty unacknowledged, and
2. Include assumptions without acknowledging them as such.
It is perfectly acceptable to be uncertain (in fact it is required in most investigations). It is also perfectly acceptable to include assumptions within an investigation. What is not acceptable, from a regulatory and patient safety standpoint, however, is to pretend that these inclusions are as good as true (or scientifically justified in the same category as fact)! Nope. These are in separate categories, each carrying different weight when it comes time for the final decision to be made. This is a critical fault that we see regularly cited in FDA Form 483s, with wording such as failure to provide “scientific rationale” for the ultimate conclusion & CAPA. Modern QRM tools take all the subjectivity encountered during the course of the investigation and force us to acknowledge what we don’t know. As a result, brilliantly, we can take the subjectivity out of the final conclusion & CAPA. That is how we can deal with uncertainty and assumptions while still ensuring patient safety. Very cool.
ICH Q9 (R1) states that “While subjectivity cannot be completely eliminated from quality risk management activities, it may be controlled by addressing bias and assumptions, the proper use of quality risk management tools and maximizing the use of relevant data and sources of knowledge (see ICH Q10, Section 1.6.1).”
“All participants involved with quality risk management activities should acknowledge, anticipate, and address the potential for subjectivity.”
In conclusion, and as a friendly reminder, transparency is always rewarded in the end. It takes practice and the right tools, but lucky for us, the roadmap for success has already been drawn through harmonized guidance.
Join us this May as we discuss, debate, and work through real-life case studies with the central theme of conducting thorough & scientific investigations that will pass any regulatory scrutiny, and ultimately ensure safety of our patients despite the inevitable: unexpected events.
Let’s go!
Pete
March 21st , 2023
Sources of Variability
If someone this afternoon forced me to propose one concept/hot topic to focus on based on recent 483s (and warning letters), both in the clinical and commercial GXP space, I would have to settle on “understanding sources of variability” in your end-to-end process, whatever GXP process that may be. Sources of variability can be defined as steps along a data collection -> review -> reporting process where hazards (see the revised ICH Q9 R1) exist that could affect the scientific justification for the ultimate decision-making step. Generally, these fall into one of two categories:
Technical Hazards (e.g., system-system interface)
Procedural Hazards (e.g., access to edit the contents of a report template)
In the PIC/s Guide for Data Integrity, we find an entire section dedicated to “hybrid systems”: those process that involve computerized systems that may not be fully complaint with regulatory expectations (e.g., simple laboratory instrumentation). These are obvious sources of variability within our manufacturing/testing processes due to reliance on procedural/human controls that need to be well understood and monitored appropriately. This is covered in the PIC/s Guide – and should be well understood in industry.
In reality, however, in 2023 and for the foreseeable future, nearly all of our processes are actually in some way “hybrid”, even if the computerized system is “compliant” with the requirements found in Part/Annex 11. I can think of few GXP processes (collection -> review -> reporting) that are truly automated. Most of the data & metadata that eventually make it to the decision-making step involve several hazards downstream from the “original” record. Even those that are mostly automated, involve at least some human intervention along the way, like the printing of a batch report following completion of an aseptic fill.
In pharma, we find it hard to be transparent with all procedural hazards. In my opinion, this is due to the serious nature of the trials we conduct and products we manufacture. Our processes have direct health and safety implications to potentially millions of our fellow humans. To admit that a hazard in our process is due to an employee failing to print and attach all filter integrity results (despite significant training and education) is difficult. This is due to the universal human condition called “cognitive dissonance”: defined as the discomfort that one experiences when dealing with a conflict between our beliefs and reality. To avoid the discomfort (extreme in our case), sometimes we choose to ignore reality. Let’s break it down:
Belief: Employees working in a GXP environment understand the serious nature of their roles and responsibilities, and will act with integrity while performing their day-to-day functions.
Reality: Employees do understand the serious nature of their roles and responsibilities, however, can only work with the tools available to them within the GXP workplace. Ultimately, the need for personal wellbeing (financial, mental, etc.) will overcome requirements of the GXP workplace.
This second point is extremely uncomfortable – that’s the cognitive dissonance kicking in.
Hence – “understanding sources of variability”. In the preamble to 21 CFR Part 11, published on March 20, 1997 (nearly 26 years ago exactly!) states “the agency’s experience with various types of records and signature falsification demonstrates that some people do falsify information under certain circumstances”. The Agency is not making a statement disparaging the GXP workforce. On the contrary! The Agency is pushing management to acknowledge Reality & the universal human condition. It’s OK to have processes that are not perfect, and sometimes under pressure, humans act in ways that they would not otherwise consider. If we are aiming for true process control, acknowledging the human condition in our data governance strategies gets us as close to perfection as possible.
Let’s do it.
Pete
March 10th , 2023
GCP Data Integrity
(EMA 2023)
I just finished reading the newly published EMA guideline titled: “Guideline on computerised systems and electronic data in clinical trials”. I think I have now transformed into a total data nerd, because I found myself completely engrossed in the text! My first thought was one of relief: I found the guide to be 100% harmonized with the many existing GXP guides for data integrity. We will not find in the document a prescribed checklist to follow when setting up or evaluating a trial management strategy. This is by design. Checklists lead to trouble! We are the experts in our data processes, and only we have the ability to design a risk-based management strategy that meets our patient expectations!
We do (at least) see an excellent high level critical-thinking roadmap to success (Section 4) for inspection readiness (via patient protection), some thoughts on which are outlined below:
1. Data Integrity
The guideline uses the concept of data governance to ensure data integrity. This is a necessary addition, as governance focuses industry on the process (a wholistic approach), rather than just the people!
2. Responsibilities
In this section we see an emphasis on data ownership (although that exact terminology is not used). When ownership is assigned, required tasks get done!
3. Context
Here we see the regulator explain that metadata provides the context necessary to generate information. Data by itself (without the associated context) cannot be used for decision-making. Only by including the associated metadata in the governance strategy can we generate information used for making decisions and conclusions (for example, by ensuring via Audit Trails that the data entry was made by the authorized employee, at the designated timepoint, etc…).
4. Source Data
This is an excellent section that outlines the ability to take a risk-based approach to ensuring accuracy of our data. Here is where we see a break from downstream GMP requirements for “original records”, however, this will most likely be adapted within the GMP framework as we move into more advanced data analytics (e.g. machine learning).
5. Criticality & Risks
To wrap up the emphasis on governance, the guide directs us over to the concepts outlined in ICH Q9 (R1) – with an almost cut/paste strategy!
6. Data Capture
Due to the wide variety of data acquisition tools that may be involved in a study, the regulators state that a “detailed diagram” of the data flow should be available. This is excellent guidance and is not optional (see the section on data integrity above), as the data & process map is the best tool to initiate process understanding, with the ultimate goal of true governance.
7. Electronic Signatures
This section is a reminder regarding the requirements for e-sigs, the reason being that without these safeguards in place, the regulator cannot consider the resulting decisions to be based on accurate and complete data sets. Just a friendly reminder!
8. Data Protection
Confidentiality of subject data cannot be compromised. The regulator includes here a section on GDPR to ensure that the risk-based governance plan considers confidentiality and implements controls that are commensurate with this risk. This is not optional!
9. Validation
To understand the roadmap at this point, we are directed to Annex 2 of the document, which is an extensive guide to CSV. We see alignment here with FDA’s 2018 DI guidance, with an emphasis on evaluating hardware, software, personnel and documentation as part of the validation process (see section A2.3). We also see some limited aspects of an Agile approach to validation (see section A2.5), following a risk-based approach. In summary, this section is a brief summary of an expected modern approach to GXP validation lifecycle.
10. Direct access
This section (in my opinion) may be a prelude to the expectation that inspectors be provided remote access to GXP data sets (read-only access), as the regulators attempt to reduce travel burden and improve efficiency through remote evaluations.
Section 5 and 6 get down into the weeds Computerised Systems (5) and Electronic Data (6), largely harmonized with Part/Annex 11 expectations. Pay special attention to section 6.2, as it outlines some very specific inspector expectations regarding Audit Trails, for example, the ability to export the “entire audit trail as a dymamic data file”… This means the inspector expects to receive an exported data file with the ability to sort/filter/process the data during inspection (data analytics). It appears that the days of providing exported PDFs are over, as this is not in a usable format and the inspector has no ability to perform their job of protecting and promoting public health.
In summary, this is another excellent harmonized GXP guide for industry with some additional specific requirements for the BIMO world. The takeaway message, as with all recent DI guides, is to:
1. Activate critical thinking and be open to flexible data management strategies (perfection is not the goal)
2. Each step and interface within a process must be evaluated for hazards/risks (think accuracy and completeness)
3. When relevant aspects of the design/operation/monitoring of the process have been evaluated and the management strategy decided, we are now operating within a validated state – and are inspection ready!
Let’s get to it!
Pete
February 23rd , 2023
Root Cause Analysis
The “5 M’s” or sometimes known as the “Fishbone (Ishikawa) Diagram” is an excellent tool for performing a structured root cause analysis (RCA), and is found in many GXP investigations. I have seen it used all over the world, with varying degrees of success when it comes to finding the root cause(s) in the context of an issue (say: deviation) potentially affecting patient safety. For the sake of this blog, let’s take a step back for a moment and gain some perspective… When we gain perspective, we are then able to think critically and act decisively. Without perspective, sometimes we get lost in the mundane world of “compliance” and act without clear direction. So:
Q: Why do we do GXP root cause analysis?
A: To identify the source(s) of the (deviation), to set us up for proposing a meaningful and effective CAPA. In theory, this prevents re-occurrence of the event.
Great, I think we can all agree with the above thought process, it’s simple and universal. So why is it then, that despite the widespread use of this tool, we continue to see repeating issues within our organizations that often demonstrate an unacceptable trend during Health Authority inspection? Maybe, it is due to lack of perspective leading to failure to use the tool to the best of its ability. A “compliance mindset” puts pressure on personnel to find the root cause within a pre-defined timeframe (typically 30 days) and lose the perspective that drive us to do the best we can with what we have. We try to fit a square peg through a
The goal with any RCA tool used in a GXP setting is to trigger critical thinking by the user. Facilitating a dedicated workshop session to the use of the tool and expanding the SOPs to include model examples are easy improvements to achieve this goal. But, if we are being serious, this isn’t going to do much, otherwise this blog entry would not be necessary. What we really need is a paradigm shift in the way RCA is done in our industry – which (in my opinion) starts by taking the advice of the FDA written in many recent Warning Letters (since ~2019): focus on the “management strategy”. RCA outcomes are only as good as the tools available. We can’t expect industry leading investigations when our tools are not kept up to date with CGMP expectations! There is a reason why the regulators are pointing us in this direction, as we see in ICH Q10:
“Senior management has the ultimate responsibility to ensure an effective pharmaceutical quality system is in place to achieve the quality objectives, and that roles, responsibilities, and authorities are defined, communicated, and implemented throughout the company.”
So if no one is evaluating the effectiveness of the abovementioned expectations, then maybe we have lost perspective? Chasing our tails with layer upon layer of CAPAs which generally increase burden on front line employees and decrease the “right environment”…
There are two ways I see this getting done (evaluating the management strategy using our RCA tools):
1. Transform 5 M’s into 6 M’s, with the addition of “Management Strategy”
a. Although this is listed as the first option, it may not be ideal in some cases. For sites with a long history of operations, the addition of the extra branch might be necessary to ensure a change (old habits die hard), however, for new sites, management strategy can be integrated into the personnel branch right from the beginning.
2. For major/critical investigations, apply a secondary RCA tool once the fishbone is completed – the “5-whys” – with a special emphasis on examining the current management strategy and “why” the event was allowed to occur in the first place.
a. For example:
i. Why has management failed to invest sufficient resources?
ii. Why did our leading Quality Indicators fail to adjust the process before failure?
b. For further guidance on this point, check out the “Right Environment” concept within MHRA’s Data Integrity guide.
RCA is no walk in the park, and it takes a bold team of individuals within management to be open to honest evaluation (= vulnerability), but when we take a step back and gain perspective (why we do what we do), we see clearly that a true Quality Culture (and ultimately the patient) would expect nothing less. Without this deeper evaluation, we might imagine a cook tasked with preparing a gourmet meal, but only provided canned ingredients – it is a guaranteed failure. In essence, it is a guarantee that we will continue to see adverse trends if we do not adjust the tools (or ingredients!).
The culture that exists within an organization when management expresses vulnerability by reacting to what the data tells us (even if it means admitting our original efforts were wrong) is one that fosters growth and will emerge in the future as an industry leader.
Oh and BTW – is a workplace where employees thrive, and find meaning in labor. Very cool.
Let’s get to it.
Pete
It appears that lately, the idea of Quality Intelligence has been a topic of growing interest among industry and the regulators. The concept should not be new to us, as the concept was originally introduced along with FDA Process Validation guidance more than 10 years ago as “Stage 3” continuous process verification (CPV). We may now be seeing more regulatory enforcement in this area, as regulators work hard to push companies to prevent the quality and manufacturing issues behind 62% of drug shortages in the United States. One recent, expertly written 483, for example, linked downstream re-occurring QC investigations with an upstream failure to evaluate “inter- and intra-batch variability” during process validation. As far as I can tell, this is new 483 language, and exactly what the patient expects.
Prevention of problems can only be fully realized when a site takes the gigabytes (terabytes?) of data they are required to retain as information, and translate them into “knowledge”. That sentence was easy for me to write… but is much more difficult for a site to “do”. As one of my heroes W. Edwards Deming would say, “by what means”? This is where things get tricky, but also (at least for me) is the fun part! Does a modern “Stage 3” CPV simply consist of continuously updated control charts with our CPPs & CQAs (and perhaps some other application commitment data points)? Nope.
What is knowledge?: GXP data/metadata/information becomes knowledge once put in the context of patient safety. It really is as simple as that.
By first understanding our processes, specifically sources of variability arising from:
· software & hardware,
· facilities & equipment,
· and personnel & documentation (see ICH Q9),
we can design a modern Quality Intelligence approach that takes available information behind sources of variability and works to reduce variation by acting on knowledge. This allows us to step off the treadmill (we are tired anyhow), and break through the barriers that prevent us from achieving a world-class manufacturing & testing facility.
Let’s get to it!
Pete
February 10th , 2023
Quality Intelligence
The GEMBA walk is an important ingredient to the pharmaceutical process control strategy and/or data governance strategy. The GEMBA walk, as it was originally intended, exists to establish a direct line of communication/visibility between upper management and front-line employees. How can upper management make critical steering decisions based on hearsay? – it is inefficient and risky! This very cool concept was designed to identify sources of variability that lead to excessive waste, which causes increased costs, a reduction in quality, and worker frustration. It is accomplished by listening, collaborating, and making corrections where improvements are needed. Not inspecting, examining, or interrogating; this kind of behavior works contrary to the goals of the program as it is management by fear.
The GEMBA, if conducted in the right spirit, can be a form of spontaneous brainstorming that can add incredible process improvements. It is simply human nature that sometimes those involved in the day-to-day activities (front-line) or managing the day-to-day activities (middle management) are too invested in the process themselves to notice these opportunities.
I have observed some additional benefits of the GEMBA walk, that I would like to share here:
1. Upper management on the shop floor demonstrates that communication is essential, which motivates middle management to perform their essential role: create the “right environment” for employees (see MHRAs DI guidance). Some even call this a “speak up culture”.
2. Upper management on the shop floor listening to employees with several layers of middle management between them demonstrates that everyone participates in quality, and old-school quality metrics goals (e.g. reduction of deviations through “re-training”) are now fossilized deep underground, never to be misused again through management by fear. We now measure performance of the process, and value everyone’s efforts to reduce sources of variation.
Quality culture gimmicks are fun (t-shirts, games, etc.), and are a welcome break from our routine activities. But what to employees really need in order to thrive both personally and professionally? Meaning in Labor. Feeling Valued. Helping Others.
The products we produce make these goals easy to achieve. Let’s get to it!
Pete
January 16th, 2023
The GEMBA